- Clinical Technology
- Adult Immunization
- Hepatology
- Pediatric Immunization
- Screening
- Psychiatry
- Allergy
- Women's Health
- Cardiology
- Pediatrics
- Dermatology
- Endocrinology
- Pain Management
- Gastroenterology
- Infectious Disease
- Obesity Medicine
- Rheumatology
- Nephrology
- Neurology
- Pulmonology
Pulmonary involvement in a patient with lymphocytic colitis
Microscopic colitis is a noninfectiouscolitis that is characterizedby chronic nonbloodydiarrhea and macroscopicallynormal colonic mucosa. Extraintestinalmanifestationsare rarely seen. In this report,we describe a nonspecific interstitialpneumonitis in a patientwith lymphocytic colitis.
Microscopic colitis is a noninfectious colitis that is characterized by chronic nonbloody diarrhea and macroscopically normal colonic mucosa. Extraintestinal manifestations are rarely seen. In this report, we describe a nonspecific interstitial pneumonitis in a patient with lymphocytic colitis.
Microscopic colitis is a distinct form of noninfectious inflammatory colitis that is characterized by chronic, watery diarrhea and a macroscopically normal colonic mucosa. Two types of microscopic colitis have been identified based on histopathological characteristics: lymphocytic colitis and collagenous colitis. Lymphocytic colitis is characterized by an increased number of intraepithelial lymphocytes.1,2 A diffuse and thickened subepithelial collagen layer is seen in patients with collagenous colitis.
In contrast to ulcerative colitis and Crohn disease, extraintestinal manifestations are uncommon inmicroscopic colitis. Pulmonary involvement is extremely rare. Wiener3 described a case of pulmonary fibrosis diagnosed by open lung biopsy in a patient with collagenous colitis. However, the author suggested that the pulmonary involvement could be a part of systemic disease. In this case, the patienthad been treated with sulfasalazine.3 Since sulfasalazine is well known to cause pulmonary toxicity, the interstitial pneumonitis and fibrosis may have been the result of a drug reaction.
We describe a patient with lymphocytic colitis who presented with dyspnea and cough. Nonspecific interstitial pneumonitis (NSIP) was found on lung biopsy. To the best of our knowledge, this is the first reported case of NSIP in a patient with lymphocytic colitis.
The case
A 69-year-old woman presented with chronic diarrhea, dry cough, and progressive dyspnea. Nonbloody diarrhea associated with low-grade fever developed approximately 3 months before presentation. She had no abdominal pain, nausea, vomiting, heartburn, tenesmus, or jaundice. Two months before presentation, the patient experienced worsening cough, progressive dyspnea, and worsening diarrhea. She also reported night sweats and a 5.5-kg (12-lb) weight loss over 2 months.
The patient's medical history was significant for hypercholesterolemia, which was treated with atorvastatin for 2 years. She was a lifelong nonsmoker. Seven months before presentation, she had visited China. A detailed exposure history was unrevealing.
On presentation, physical examination revealed a temperature of 39.5°C (103.1°F), blood pressure of 122/70 mm Hg, heart rate of 89 beats per minute, and respiration rate of 17 breaths per minute. Oxygen saturation while breathing ambient air was 90%. There were no palpable lymph nodes. Chest auscultation showed bilateral scattered crackles. Findings on skin, cardiac, and abdominal examinations were unremarkable. Clubbing of the fingers and toes was absent.
Initial laboratory findings included a white blood cell count of 10.1 × 103/µL, hemoglobin level of 14 g/dL, platelet count of 247 × 103/µL, normal serum chemistry panel, creatinine level of 0.9 mg/dL, and normal liver transaminase levels. Blood cultures and stool cultures were negative for bacterial pathogens. Three stool samples were negative for white blood cells, ova, and parasites. Two stool samples were negative for Clostridium difficile toxin. Serological test results were negative for Yersinia. Arterial blood gas analysis showed a Po2 of 46 mm Hg while breathing ambient air.
A chest radiograph obtained 2 weeks before presentation showed mild increased interstitial markings and hyperinflation (Figure 1A). A chest radiograph obtained on presentation showed new bilateral pulmonary infiltrates (Figure 1B). A CT scan of the chest showed diffuse bilateral ground-glass infiltrates (Figure 2).
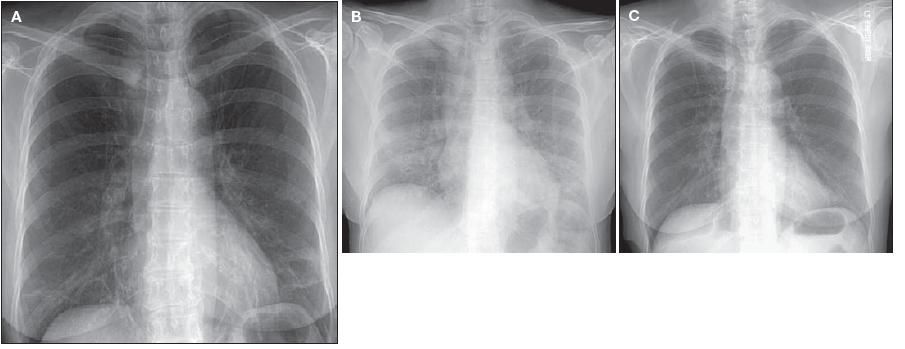
Figure 1 – A chest radiograph obtained 2 weeks before presentation showed a mild increase in interstitial markings and hyperinflation (A). On presentation, the chest radiograph showed new bilateral pulmonary infiltrates (B). Treatment with prednisone resulted in resolution of the pulmonary infiltrates (C).
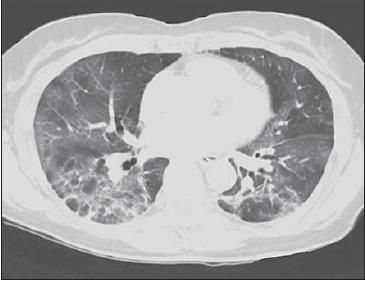
Figure 2 – CT scan of the chest revealed diffuse bilateral ground-glass infiltrates.
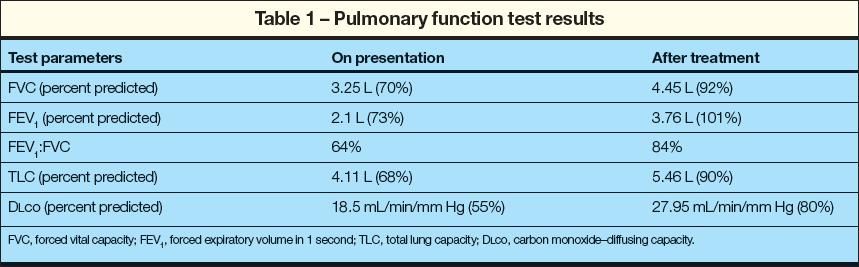
Bronchoscopy with bronchoalveolar lavage (BAL) was performed. Findings from cytological examination of BAL fluid were unremarkable. The differential cell count revealed 44% macrophages, 39% lymphocytes, 12% neutrophils, and 5% eosinophils. Cultures of BAL fluid were negative for bacteria, mycobacteria, viruses, and fungi. The results of urinary antigen testing for Legionella were negative. Pulmonary function testing showed low lung volumes, mild obstruction, and markedly reduced carbon monoxide–diffusing capacity (Table 1).
Colonoscopy showed normal mucosa. Several random biopsies of mucosa from the entire colon were performed. The pathology showed inflammation of lamina propria with intraepithelial lymphocytes (more than 20 lymphocytes per 100 epithelial cells), which is consistent with the diagnosis of lymphocytic colitis.
An open lung biopsy was performed. The pathological examination of the lung biopsy specimen showed NSIP (Figure 3). Immune staining revealed no immune complexes or complement component in the lung tissue. These pathological findings suggested the presence of interstitial pneumonitis and fibrosis secondary to a pauci-immune lymphocytic alveolitis.
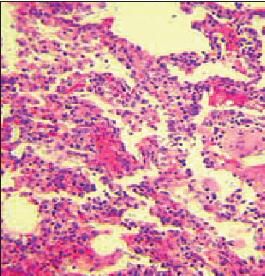
Figure 3 –
Lung biopsy identified interstitial pneumonitis (hematoxylin and eosin stain, ×40).
The patient was given oral prednisone, 40 mg daily. After 4 weeks of prednisone therapy, she reported marked improvement in diarrhea and dyspnea. A chest radiograph was repeated, and it showed resolution of the pulmonary infiltrates (Figure 1C). Marked improvement in pulmonary function test results was also noted.
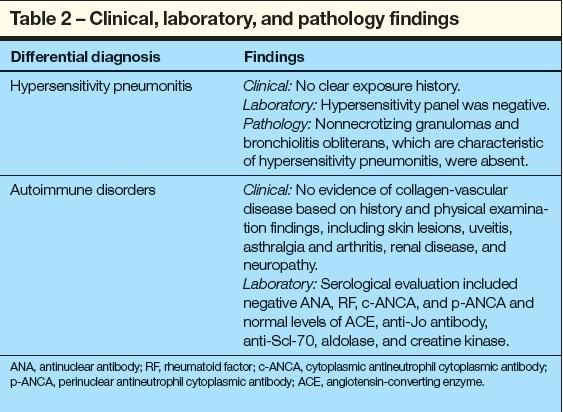
Further workup showed no other cause of NSIP.Table 2 summarizes the laboratory findings.
Discussion
NSIP is an interstitial pneumonitis that does not conform to the characteristic features of other interstitial lung diseases, including usual interstitial pneumonitis (UIP), desquamative interstitial pneumonitis,organizing pneumonia, acute interstitial pneumonitis, and respiratory bronchiolitis–interstitial lung disease. It is characterized pathologically by homogeneous and diffuse chronic interstitial inflammation, dense or loose interstitial fibrosis lacking the temporal heterogeneity and patchy distribution characteristic of UIP, and preserved lung architecture.4,5
NSIP can occur in a wide variety of clinical settings, such as collagen- vascular disease; drug reactions; inhalation of organic dust; resolving acute lung injury or infections; and inadequately sampled UIP, hypersensitivity pneumonitis, or organizing pneumonia. However, in the case presented here, the history, physical examination, and laboratory findings did not reveal any evidence of another disease process.
Hypersensitivity pneumonitis should be included in the differential diagnosis of NSIP; the 2 entities share some histopathological criteria. However, other characteristic pathological findings of hypersensitivity pneumonitis, including peribronchiolar accentuation, non-necrotizing granulomas, and bronchiolitis obliterans, were absent in the case presented here.6 NSIP secondary to inhalational injury was excluded on the basis of a detailed history.5
Rheumatological disorders also have been associated with an NSIP pattern lung injury.5 Rare cases of celiac disease and NSIP have been described. The negative results of serum IgA endomysial antibody, IgA tissue transglutaminase antibody, and antigliadin antibodies strongly argued against the presence of celiac disease in the patient we described above.7
Interstitial pneumonitis is a well-known extraintestinal complication of ulcerative colitis and Crohn disease.8 Ulcerative colitis and Crohn disease were excluded by the findings from colonoscopy and colonic mucosa pathology.
NSIP also is seen in pulmonary drug toxicities.5 Our patient had been receiving atorvastatin therapy for 2 years. Although pulmonary toxicity has been reported with simvastatin,9 atorvastatin lung toxicity has not been described. The patient improved despite continuation of this therapy. Because the clinical course of the pulmonary disease was not influenced by exposure to (or continuation of) atorvastatin, we concluded that this agent was an unlikely cause of NSIP in our patient.
The cause of microscopic colitis is not known. Two possible mechanisms have been proposed: autoimmune response and induction by medications.10 Additional diseases with a presumed autoimmune cause are present in 40% to 45% of patients with microscopic colitis. Celiac sprue, autoimmune thyroiditis, psoriasis, polymyalgia rheumatica, and rheumatoid arthritis have been associated with microscopic colitis.1,2,10
Systemic symptoms, such as fever, weight loss, arthralgia, and spondylopathy, are infrequently seen in microscopic colitis, and their presence suggests a systemic inflammatory process.11,12 NSIP is a commonly seen lung injury pattern in autoimmune diseases. It is possible that our patient's disease process was a result of the activation of lymphocytes to an undetermined auto-antigen shared by the lungs and colon.
Medications are also associated with development of microscopic colitis. For example, the platelet activation inhibitor ticlopidine has been associated with development of microscopic colitis and pulmonary involvement. Persoz and associates13 described a case of microscopic colitis and pulmonary involvement in a patient treated with ticlopidine for transient ischemic cerebrovascular accidents. The patient had bilateral pulmonary infiltrates and a restrictive defect shown on pulmonary function testing. Bronchoscopy showed lymphocytic BAL fluid. No biopsy was done. The pulmonary disease and colitis improved with prednisone and the withdrawal of ticlopidine.13
Our case also suggests colon and lung injury secondary to a lymphocytic process. We believe our patient had NSIP associated with lymphocytic colitis. Similar to ulcerative colitis and Crohn disease, interstitial pneumonitis may represent a rare systemic manifestation of lymphocytic colitis.
References:
REFERENCES
1.
Olesen M, Eriksson S, Bohr J, et al. Lymphocytic colitis: a retrospective clinical study of 199 Swedish patients.
Gut.
2004;53:536-541.
2.
Barta Z, Mekkel G, CsÃpo I, et al. Microscopic colitis: a retrospective study of clinical presentation in 53 patients.
World J Gastroenterol.
2005;11:1351-1355.
3.
Wiener MD. Collagenous colitis and pulmonary fibrosis. Manifestations of a single disease?
J Clin Gasteroenterol.
1986;8:677-680.
4.
Katzenstein AL, Fiorelli RF. Nonspecific interstitial pneumonia/fibrosis. Histologic features and clinical significance.
Am J Surg Pathol.
1994;18:136-147.
5.
Leslie KO. Pathology of interstitial lung disease.
Clin Chest Med.
2004;25:657-703.
6.
Selman M. Hypersensitivity pneumonitis: a multifaceted deceiving disorder.
Clin Chest Med.
2004;25:531-547.
7.
Ben-Bassat O, Lev S, Gafter-Gvili A, et al. Acute pneumonitis in a patient with celiac disease and dermatitis herpetiformis.
Isr Med Assoc J.
2005;7:340-341.
8.
Camus P, Piard F, Ashcroft T, et al. The lung in inflammatory bowel disease.
Medicine (Baltimore).
1993;72:151-183.
9.
Lantuejoul S, Brambilla E, Brambilla C, Devouassoux G. Statin-induced fibrotic nonspecific interstitial pneumonia.
Eur Respir J.
2002; 19:577-580.
10.
Holstein A, Burmeister J, Plaschkle A, et al. Autoantibody profiles in microscopic colitis.
J Gastroenterol Hepatol.
2006;21:1016-1020.
11.
Cacoub P, Sbai A, Toan SV, et al. Collagenous colitis. A study of 11 cases [in French].
Ann Med Interne (Paris).
2001;152:299-303.
12.
Narváez J, Montala N, Busquets-Pérez N, et al. Collagenous colitis and spondylarthropathy.
Arthritis Rheum.
2006;55:507-512.
13.
Persoz CF, Cornella F, Kaeser P, Rochat T. Ticlopidine-induced interstitial pulmonary disease: a case report.
Chest.
2001;119:1963-1965.
