- Clinical Technology
- Adult Immunization
- Hepatology
- Pediatric Immunization
- Screening
- Psychiatry
- Allergy
- Women's Health
- Cardiology
- Pediatrics
- Dermatology
- Endocrinology
- Pain Management
- Gastroenterology
- Infectious Disease
- Obesity Medicine
- Rheumatology
- Nephrology
- Neurology
- Pulmonology
Lung nodules as the first manifestation of Crohn disease
A 19-year-old woman presented with shortness of breath, dry cough, and pleuritic chest pain of unknown duration. Her medical history included endometriosis, a benign ovarian cyst,
The case
A 19-year-old woman presented with shortness of breath, dry cough, and pleuritic chest pain of unknown duration. Her medical history included endometriosis, a benign ovarian cyst, and nonspecific chest discomfort with occasional dyspnea on exertion several months earlier. There were no previous hospitalizations or significant family history.
The patient denied fever, night sweats, productive cough, hemoptysis, wheezing, orthopnea, cyanosis, rhinorrhea, sinusitis, travel outside of her home state (Illinois), exposure to tuberculosis, exposure to birds, and injection drug use. She was allergic to milk but had no other allergies. She was a college student, lived alone, worked in sales, and smoked 10 to 12 cigarettes per day for 2 years. She admitted to occasional social alcohol intake. The only medication she took was medroxyprogesterone.
Physical examination revealed a well-developed and well-nourished woman with pallor, mild tachypnea, low-grade fever, and white sclerae. The patient reported right lower pleuritic chest pain on deep inspiration. Findings from the rest of the physical examination were not remarkable.
The differential leukocyte counts and hemogram, urinalysis, and blood chemistry results were normal. Erythrocyte sedimentation rate was 81 mm/h. The results of serum angiotensin-1–converting enzyme, antinuclear antibody, antineutrophilic cytoplasmic antibody tests; a purified protein derivative skin test; chest radiography; and bronchoscopy were normal.
However, a CT scan of the chest displayed 2 right upper lobe nodules about 2 cm and 1 cm in diameter (Figure 1). The rest of the lung parenchyma and vasculature and the mediastinum were normal. The results of a CT-guided fine-needle aspiration biopsy of the lung lesions were nondiagnostic. Bacterial and fungal cultures were negative for organisms.

Figure 1 – Two discrete nodules are demonstrated in the right upper lung parenchyma on this CT scan.
Subsequent wedge resection of the 2 right upper lobe nodules was tolerated well. Microscopically, the lesions were interpreted as noncaseous granulomata and bronchiolitis obliterans with organizing pneumonia (BOOP) (Figure 2). The microbial culture was negative for identifiable microorganisms; periodic acid-Schiff stain, methenamine-silver stain, and Fite-Farraco procedure also failed to show discernible microorganisms.
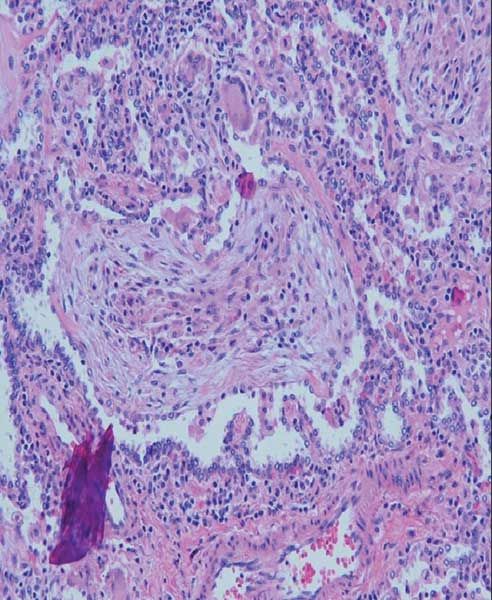
Figure 2 – Granulomata and bronchiolitis obliterans with organizing pneumonia are prominent microscopy findings (hematoxylin and eosin stain, ×100).
One month after thoracotomy, the patient presented with acute abdominal pain associated with nonspecific abdominal discomfort, diarrhea, and a few episodes of some blood in her stools. Her abdomen was soft and symmetrical without pain or tenderness. No costovertebral angle or spine tenderness was elicited.
Radiographic imaging demonstrated apparent pneumoperitoneum; a small amount of free intra-abdominal fluid; normal visceral organs; transverse colon perforation; and rectouterine air-fluid collection, consistent with an abscess. Exploratory laparotomy and segmental resection of the large intestine grossly and microscopically demonstrated Crohn disease (Figure 3). The patient’s postoperative course was uncomplicated, and there was no recurrence of lung or intestinal Crohn disease at 60 months’ follow-up.

Figure 3 – A cobblestone mucosa with serpentiginous ulcers of Crohn disease is striking in the resected enteric segment.
DISCUSSION
The diagnosis of chronic inflammatory bowel disease (IBD), which includes ulcerative colitis and Crohn disease, is sometimes preceded by various extraintestinal manifestations. These may include respiratory and other systemic complications. The paucity of literature on this topic is rather remarkable, considering that IBD is fairly common.1-9
Pulmonary manifestations of IBD were originally reported in 1976 in 6 patients who presented with chronic purulent sputum. Pulmonary involvement is uncommon in IBD, probably because of underreporting. In patients with IBD who have respiratory complaints, chest radiographic findings are often normal; as a result, clinical workup is not pursued. Moreover, respiratory involvement associated with IBD may occur many years after enterocolectomy and resolution of bowel symptoms; therefore, it may be difficult to prove the relationship between the two.1-9 The pulmonary symptoms may precede the intestinal disease, as in our patient.
Bronchial involvement is the most common pulmonary manifestation in IBD, but other presentations may include upper airway disease, parenchymal infiltrates, and serositis. The lung lesions are usually consistent with BOOP and interstitial disease and are more commonly described with ulcerative colitis than with Crohn disease. There is a female predominance of almost 2:1 for bronchopulmonary problems and up to 4:1 for airway complications alone. In contrast, serositis occurs with roughly equal frequency in men and women.1-9
Airway complications may follow the onset of IBD in 80% to 85% of patients, precede IBD in 10% to 15%, and develop concomitantly in 5% to 10%. Serositis generally manifests during episodes of active IBD, and parenchymal lung disease commonly occurs during quiescence.1-9
The pathogenesis of the pulmonary parenchymal disease and serositis is unknown. However, the more common airway inflammatory changes have been thought to mimic the inflammatory changes that occur in the bowel. The upper airways also may reveal subglottic inflammation and stenosis. The bronchial involvement appears as chronic bronchitis or bronchiectasis. The findings on a chest radiograph may be normal, but a CT scan may show bronchial wall thickening, dilated airways, and mucoid impaction.
The small-airway involvement may be characterized by granulomatous bronchiolitis. In serositis (pleural effusions, pericarditis, pleuropericarditis, and myopericarditis), the fluid is exudative and cell content is primarily neutrophilic.1-9
Recent data have focused on treatment-related adverse effects, such as alveolitis and pneumonitis, with the use of sulfasalazine, mesalamine (5-aminosalicylic acid), methotrexate, and azathioprine.1 The large-airway disease is more responsive to treatment than is bronchiolitis. The delivery of inhaled corticosteroids (such as beclomethasone, 1.5 to 2 mg/d) to small airways is known to be relatively poor. Subglottic involvement that causes obstruction may require intravenous corticosteroids.
Pulmonary parenchymal complications of IBD may have to be treated with oral corticosteroids; prednisone is initially given at a dosage of 0.5 to 1 mg/kg/d. Most likely, treatment will be needed for several months. Serositis and pleural effusions, especially if symptomatic, are managed with NSAIDs and corticosteroids.1-9
References:
REFERENCES1. Sharma S, Eschun G. What are the pulmonary manifestations of inflammatory bowel disease? J Respir Dis. 2007;28:227-234.
2. Coonar AS, Hwang DM, Darling G. Pulmonary involvement in inflammatory bowel disease. Ann Thorac Surg. 2007;84:1748-1750.
3. Krishnan S, Banquet A, Newman L, et al. Lung lesions in children with Crohn’s disease presenting as nonresolving pneumonias and response to infliximab therapy. Pediatrics. 2006;117:1440-1443.
4. Ahmed KA, Thompson JW, Joyner RE, Stocks RM. Airway obstruction secondary to tracheobronchial involvement of asymptomatic undiagnosed Crohn’s disease in a pediatric patient. Int J Pediatr Otorhinolaryngol. 2005;69:1003-1005.
5. Carratú P, Dragonieri S, Nocerino MC, et al. A case of cryptogenic organizing pneumonia occurring in Crohn’s disease. Can Respir J. 2005;12:437-439.
6. Freeman HJ, Davis JE, Prest ME, Lawson EJ. Granulomatous bronchiolitis with necrobiotic pulmonary nodules in Crohn’s disease. Can J Gastroenterol. 2004;18:687-690.
7. Casey MB, Tazelaar HD, Myers JL, et al. Noninfectious lung pathology in patients with Crohn’s disease. Am J Surg Pathol. 2003;27:213-219.
8. Mahadeva R, Walsh G, Flower CD, Shneerson JM. Clinical and radiological characteristics of lung disease in inflammatory bowel disease. Eur Respir J. 2000;15:41-48.
9. Hotermans G, Benard A, Guenanen H, et al. Nongranulomatous interstitial lung disease in Crohn’s disease. Eur Respir J. 1996;9:380-382.
Â
Clinical Tips for Using Antibiotics and Corticosteroids in IBD
January 5th 2013The goals of therapy for patients with inflammatory bowel disorder include inducing and maintaining a steroid-free remission, preventing and treating the complications of the disease, minimizing treatment toxicity, achieving mucosal healing, and enhancing quality of life.
