- Clinical Technology
- Adult Immunization
- Hepatology
- Pediatric Immunization
- Screening
- Psychiatry
- Allergy
- Women's Health
- Cardiology
- Pediatrics
- Dermatology
- Endocrinology
- Pain Management
- Gastroenterology
- Infectious Disease
- Obesity Medicine
- Rheumatology
- Nephrology
- Neurology
- Pulmonology
Pulmonary nocardiosis mimicking empyema necessitatis
Nocardia asteroides is a rarecause of pulmonary or disseminatedinfection in immunocompetentpersons. Pleuralcompromise is common, butempyema necessitatis is veryrare. The authors describe anapparently immunocompetentpatient with N asteroides infectionwho had chest wallcompromise mimicking empyemanecessitatis.
Nocardia asteroides is a rare cause of pulmonary or disseminated infection in immunocompetent persons. Pleural compromise is common, but empyema necessitatis is very rare. The authors describe an apparently immunocompetent patient with N asteroides infection who had chest wall compromise mimicking empyema necessitatis.
Empyema necessitatis is an empyema that extends through the parietal pleura into the adjacent tissue.1 The most common cause is tuberculosis, followed by actinomycosis and, less commonly, pulmonary infection with Streptococcus pneumoniae and atypical mycobacteria.1
Nocardia asteroides is a slow-growing, Gram-positive, partially acid-fast, ubiquitous organism that is an uncommon pathogen among immunocompetent persons. Risk factors for the development of disease include malignant tumor, transplantation, use of corticosteroids, and autoimmune disease.2
Although pleural compromise is common in pulmonary nocardiosis, chest wall fistulization is uncommon, especially in immunocompetent patients. In older case series, pleural and chest wall involvement were extrapulmonary manifestations in only 8% of patients.3 Here we describe a patient with pulmonary nocardiosis who presented with a clinical picture mimicking empyema necessitatis.
The case
The patient was a 59-year-old man admitted with an intermittent cough of 4 months' duration. The cough initially was nonproductive but became productive of bloodtinged sputum. It was accompanied by an 8-lb weight loss and a skin lesion on the anterior aspect of the left chest wall. This lesion appeared as a solitary papule, followed by 2 additional similar lesions within 1 month. The papules increased in size and became ulcerated and drained purulent fluid.
The patient denied dyspnea, fevers, night sweats, chest pain, and contact with persons with infections. He was from Mexico and had lived in the United States for 6 years. He was married, did not smoke, and denied drug use.
On admission, the patient appeared healthy. His pulse was 85 beats per minute, temperature was normal, and blood pressure was115/60 mm Hg. He was normocephalic with no oral lesions and fair dentition. On inspection, he had 3 ulcerations on the left anterior chest wall associated with surrounding hyperpigmentation, induration, and yellow discharge (Figure 1). His abdomen was soft and nontender, with no organomegaly. His extremities had no edema or additional lesions. The results of a neurological examination and the remainder of the physical examination were normal.
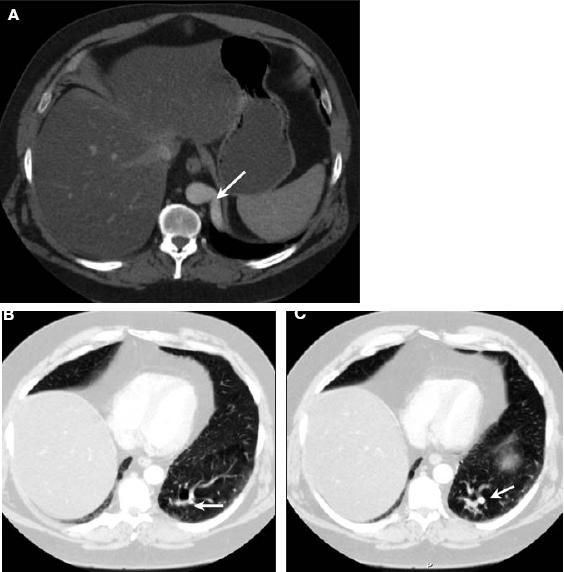
Figure 1 – These lesions appeared on the chest of a 59-year-old man who presented with intermittent cough and weight loss. The diagnostic workup confirmed nocardiosis.
Laboratory evaluation on admission revealed a white blood cell count of 13,000/μL, with 15% lymphocytes, 78% granulocytes, 1.2% eosinophils, and 5.4% monocytes; hemoglobin level of 12 g/dL; hematocrit of 37%; and a platelet count of 577,000/μL. Renal and hepatic function test results were normal, and the patient's fasting glucose level was 88 mg/dL. The results of HIV serology (by enzyme-linked immunosorbent assay), purified protein derivative skin testing, and hepatitis profile were negative.
A chest radiograph disclosed a lingular infiltrate. A CT scan revealed a soft tissue mass in the left chest wall with mediastinal lymphadenopathy (with lymph nodes up to 1.2 cm) as well as multiple small lymph nodes in the left axillary region. The complex soft tissue mass was centered on the left chest wall, extending from the skin through the subcutaneous tissue to the lingual region and then crossing the diaphragm and extending to the left upper abdomen and surrounding the pericardium (Figure 2).
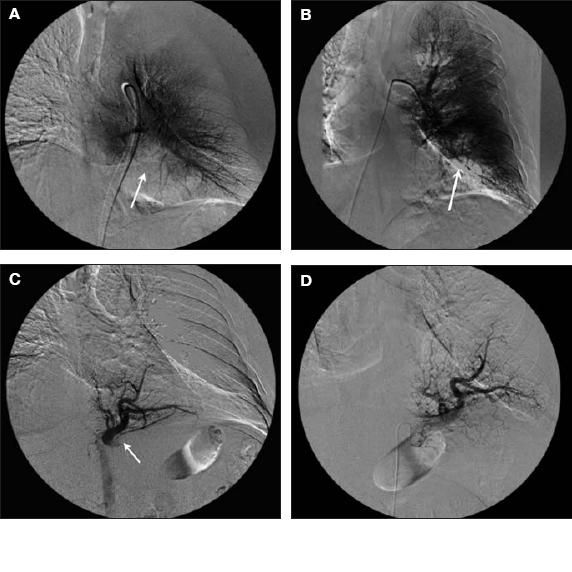
Figure 2 – A CT scan detected a complex soft tissue mass on the left chest wall, extending to the lingula and pericardium and through the diaphragm into the upper abdomen and surrounding the pericardium. This CT scan also revealed mediastinal lymphadenopathy.
Interventional radiology–guided biopsy was performed. However, the tissue was nondiagnostic and open biopsy was requested. The tissue obtained by open biopsy revealed acute and chronic inflammation with Gram-positive branching bacilli and sulfur granules consistent with Actinomyces species or Nocardia species (Figure 3).
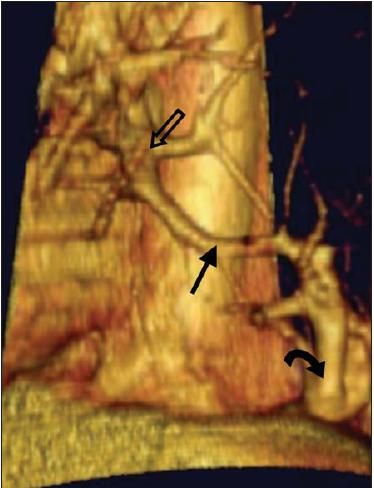
Figure 3 – Acute and chronic inflammation can be seen in these open lung biopsy specimens. The Gram-positive branching bacilli and sulfur granules are consistent with
Actinomyces
species or
Nocardia
species. Gram stain at ×100 magnification reveals multiple branching Gram-positive rods (bottom).
After 1 week of incubation, the aerobic culture was positive for a Gram-positive branching, partially acid-fast organism (Figure 4), which was later identified as N asteroides. The isolate was susceptible to ceftriaxone, amoxicillin/clavulanate, and trimethoprim/sulfamethoxazole (TMP/SMX) and was resistant to amikacin, imipenem, and tobramycin.
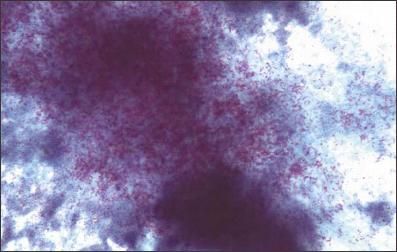
Figure 4 – This aerobic culture sample discloses a Gram-positive branching, partially acid-fast organism, which was later identified as
Nocardia asteroides.
Findings on an MRI scan of the brain were normal, and the patient was given TMP/SMX (15 mg/kg/d of trimethoprim in divided doses).
Discussion
Empyema necessitatis is an uncommon complication of pleural space infections that is typically preceded by respiratory and systemic symptoms and is followed by formation of a cutaneous nodule that eventually drains purulent material.1 Since the antibiotic era began, this clinical presentation has become extremely uncommon.1
In our patient, the indolent presentation with chest wall fistulization and the radiographic characteristics initially suggested a sarcoma. However, we also considered actinomycosis, lung cancer, tuberculosis, cryptococcosis and other endemic mycoses, bronchogenic carcinoma, and infection caused by Rhodococcus species.4,5 Furthermore, the initial appearance of the biopsy specimens suggested actinomycosis, but the positive results on acid-fast stain and growth under aerobic conditions rapidly helped clarify the diagnosis.
Nocardia is usually isolated from soil. Nocardiosis is an important infection in immunosuppressed patients. Its prevalence in the United States is estimated to be about 1000 cases per year.2
It is important to note that pleural effusion can be present in up to 35% of patients with pulmonary nocardiosis, but extension through the chest wall is uncommon.6 In a report from Spain, Julve Parvo and associates7 described the case of a 70-year-old woman with a history of diabetes mellitus who presented with pulmonary and chest wall compromise associated with destruction of the ribs-a feature that was not present in our patient. Our patient also did not have diabetes mellitus, which has been described as a risk factor for pulmonary nocardiosis.7,8
Nocardiosis seems to be more common in males than in females.2 The reason for this is not clear but may be related to hormonal factors.8 In previous reports, approximately 50% of patients did not have any apparent predisposing condition.2,3,8 Immunity against Nocardia infection depends mainly on macrophages and activated T cells, which may explain its higher incidence in HIV-infected patients and bone marrow and solid organ transplant recipients.8 Our patient did not have clinically apparent immunosuppression.
Prospective clinical trials of the treatment of Nocardia infection are lacking. Some experts advocate initial intravenous combination therapy for severe disease, followed by prolonged oral therapy.9-11 First-line therapy includes sulfa drugs, especially TMP/SMX, but minocycline is an alternative.9,10 Other agents include amikacin, cephalosporins, amoxicillin/clavulanate, fluoroquinolones, and imipenem.11 Surgical interventions such as abscess drainage and biopsies are indicated in select patients.12 In our report, the amikacin and imipenem resistance suggests an unusually resistant strain, but the patient responded well to sulfa therapy.
References:
REFERENCES
1.
Kono SA, Nauser TD. Contemporary empyema necessitatis.
Am J Med.
2007;120:303-305.
2.
Lederman ER, Crum NF. A case series and focused review of nocardiosis: clinical and microbiologic aspects.
Medicine (Baltimore).
2004;83:300-313.
3.
Palmer DL, Harvey RL, Wheeler JK. Diagnosisand therapeutic considerations in
Nocardia asteroides
infection.
Medicine (Baltimore).
1974;53:391-401.
4.
Cakir O, Topal U, Bayram AS, Tolunay S. Sarcomas: rare primary malignant tumorsof the thorax.
Diagn Interv Radiol.
2005;11:23-27.
5.
Yildiz O, Doganay M. Actinomycosis and
Nocardia
pulmonary infections.
Curr Opin Pulm Med.
2006;12:228-234.
6.
Hui CH, Au VW, Rowland K. Pulmonary nocardiosis re-visited: experience of 35 patients at diagnosis.
Respir Med.
2003;97:709-717.
7.
Julve Pardo R, Carrión Valero F, Gonzalvo Bellver F, et al. Chest wall destruction: unusual presentation form of pulmonary nocardiosis [in Spanish].
An Med Interna.
2001;18:90-92.
8.
Matulionyte R, Rohner P, Uçkay I, et al. Secular trends of nocardia infection over 15 years in a tertiary care hospital.
J Clin Pathol.
2004;57:807-812.
9.
Wilson J, Turner H, Kirchner K, et al. Nocardial infections in renal transplant recipients.
Medicine (Baltimore).
1989;68:38-57.
10.
Petersen EA, Nash ML, Mammana RB, Copeland JG. Minocycline treatment of pulmonary nocardiosis.
JAMA.
1983;250:930-932.
11.
Threlkeld SC. Hooper DC. Update on management of patients with
Nocardia
infection.
Curr Clin Top Infect Dis.
1997;17:1-23.
12.
Chazen G.
Nocardia. Infect Control.
1987;8:260-263.
