- Clinical Technology
- Adult Immunization
- Hepatology
- Pediatric Immunization
- Screening
- Psychiatry
- Allergy
- Women's Health
- Cardiology
- Pediatrics
- Dermatology
- Endocrinology
- Pain Management
- Gastroenterology
- Infectious Disease
- Obesity Medicine
- Rheumatology
- Nephrology
- Neurology
- Pulmonology
A 45-year-old man with intralobar bronchopulmonary sequestration
Bronchopulmonary sequestrationis a rare congenitallung malformation characterizedby an abnormal segmentof bronchopulmonary tissuesupplied by an anomaloussystemic artery. The diagnosismay be easily missed in adults,since many are asymptomatic;moreover, symptoms, whenpresent, often overlap withthose of other pulmonaryprocesses. Surgical resectionprovides definitive managementand is usually reservedfor patients with symptoms.We present a case of intralobarbronchopulmonary sequestrationthat presented duringadulthood.
Bronchopulmonary sequestration is a rare congenital lung malformation characterized by an abnormal segment of bronchopulmonary tissue supplied by an anomalous systemic artery. The diagnosis may be easily missed in adults, since many are asymptomatic; moreover, symptoms, when present, often overlap with those of other pulmonary processes. Surgical resection provides definitive management and is usually reserved for patients with symptoms. We present a case of intralobar bronchopulmonary sequestration that presented during adulthood.
The case
The patient was a 45-year-old man who was seen in an outpatient clinic for abdominal pain. He was obese and had obstructive sleep apnea, which was being treated with continuous positive airway pressure.
A CT scan of the abdomen failed to reveal any abnormal abdominal findings, but the lower chest cuts showed an abnormal blood vessel. The patient was subsequently referred to a pulmonary clinic.
The history and physical examination findings were unremarkable. Arterial blood gas values at rest were normal, and pulse oximetry showed no oxygen desaturation during exercise. Pulmonary function tests showed a mild restrictive defect with preserved carbon monoxide–diffusing capacity.
Findings on a CT angiogram of the chest confirmed the vascular nature of the abnormality that was seen on the abdominal CT scan, with minimal bronchoparenchymal abnormalities (Figure 1). Pulmonary and aortic angiography was performed (Figure 2). The results were as follows:
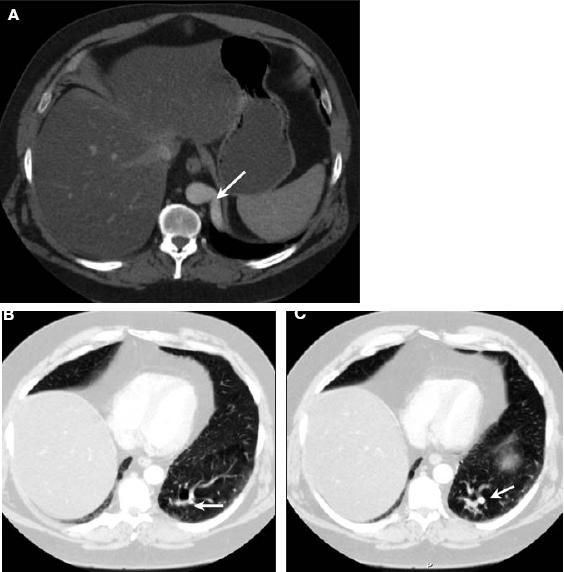
Figure 1 – CT angiogram of the chest showed an arterial feeding vessel (arrow) arising from the descending aorta within the posterior basal segment of the left lower lobe (A, B, and C). There are multiple prominent vessels, and both ground-glass and cystic changes are seen in the surrounding lung parenchyma (lung window settings, B and C).
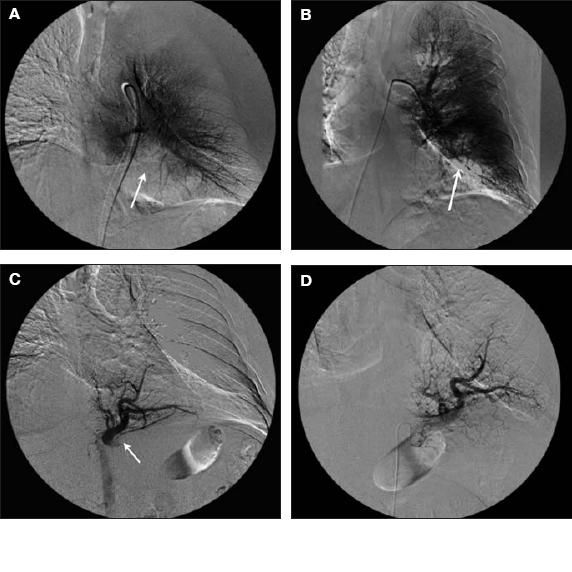
Figure 2 – Left pulmonary arteriogram shows a paucity of pulmonary arterial vessels in the left lung base posteromedially compatible with the posterior basal segment (A and B). Findings in the remainder of the left pulmonary arterial tree are unremarkable, without filling defects or other appreciable abnormality. No arteriovenous malformation or other abnormal arteriovenous shunting is identified. A descending thoracic aortogram shows the abnormal artery arising from the abdominal aorta just below the diaphragm, extending up into the basal portion of the left lung (C). A selective arteriogram of the aberrant sequestration artery shows a large vessel arising from the aorta extending up into the posteromedial and inferior portion of the left lung and filling of that segment of the lung that did not fill on the left pulmonary arteriogram (D).
• A left pulmonary arteriogram demonstrated a paucity of pulmonary arterial vessels in the left lung base posteromedially compatible with the posterior basal segment. Findings in the remainder of the left pulmonary arterial tree were unremarkable, without filling defects or other appreciable abnormalities. No arteriovenous malformation or other abnormal arteriovenous shunting was identified.
• A descending thoracic aortogram showed an abnormal artery arising from the abdominal aorta just below the diaphragm extending up into the basal portion of the left lung.
• A selective arteriogram of the aberrant sequestration artery showed a large vessel arising from the aorta extending into the posteromedial and inferior portion of the left lung and filling the segment of the lung that did not fill on the left pulmonary arteriogram. No significant arteriovenous shunting or abnormal communication between the artery and the draining left pulmonary vein was identified (Figure 3). No definite arteriovenous malformation was identified. The venous drainage was into the inferior left pulmonary vein.
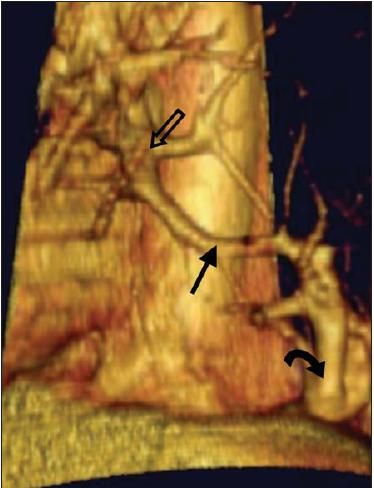
Figure 3 – This left lateral view of a 3-dimensional reconstruction of the CT scan of the chest shows the direct connection (straight solid arrow) between the aberrant artery (curved arrow) and the left pulmonary vein (hollow arrow).
• A descending thoracic aortogram more superiorly showed no other appreciable abnormalities.
These findings confirmed the diagnosis of intralobar pulmonary sequestration.
The patient did not receive any intervention. He continues to do well on follow-up visits.
Discussion
The term "sequestration" (from the Latin word "sequestrate," "to separate") was first used in the medical literature by Pryce1In 1946. Bronchopulmonary sequestration is an uncommon developmental anomaly representing only 1.5% to 6.4% of all congenital pulmonary malformations.2,3 It is characterized by abnormal, non-functioning pulmonary parenchyma that has no connection with the tracheobronchial tree and receives its blood supply from the systemic circulation. Two types of sequestration have been described: intralobar, in which the abnormal tissue is within the parenchyma of the normal lobe and does not have a separate visceral pleura, as seen in our patient; and extralobar, in which the abnormal tissue is enclosed in its own visceral pleura separate from the adjacent normal lobe.
Intralobar sequestrations represent more than 75% of sequestrations, and 60% of these are found in the posterior basal segment of the left lower lobe. Overall, 98% occur in the lower lobes. Bilateral involvement is uncommon. Unlike extralobar sequestration, intralobar sequestration is rarely associated with other developmental abnormalities. Extralobar sequestrations occur on the left side in 95% of cases. Of these, 75% are between the left hemidiaphragm and the left lower lobe.2,3
The 2 types of sequestration are associated with very different clinical features. Extralobar sequestration is typically identified in neonates because of the high frequency of concomitant congenital abnormalities. In contrast, intralobar sequestration is more likely to present later; in up to 50% of cases, the diagnosis is made after the age of 20 years. The vast majority of patients with intralobar sequestration are asymptomatic. They may carry the abnormality for years, and the diagnosis is typically made by a routine chest radiograph for unrelated symptoms.
The symptoms of intralobar sequestration are often nonspecific and can include chest pain, pleurisy, dyspnea, and wheezing; however, signs of recurrent infection, such as fever and productive cough, are more common. This risk of infection is counter intuitive, given the absence of a tracheobronchial connection to the sequestration. However, intralobar sequestrations are not completely isolated from the native lung. Bacteria can still invade via the alveolar pores of Kohn. Once bacteria have colonized the sequestration, frank infection can ensue because of the lack of normal bronchial drainage.
Although uncommon and usually benign, intralobar sequestration can present more dramatically with frank hemoptysis. There are reports in the medical literature of life-threatening hemoptysis associated with intralobar sequestration.4
The arterial supply of intralobar sequestration is a branch of the descending thoracic aorta in as many as 75% of patients. Rarely, the arterial supply comes from sites other than the aorta and has even been documented to arise from the circumflex branch of the left coronary artery.5
Because pulmonary sequestration is uncommon, it is often not considered in the differential diagnosis of a pulmonary mass in an adult. In a review of 540 cases of intralobar sequestration, the correct diagnosis was made or suspected in only 50% of the cases.2 Several fatal hemorrhages have occurred intraoperatively when aberrant vessels were transected unknowingly because the diagnosis was not established and the vascular supply not delineated preoperatively.
The diagnosis of intralobar sequestration is usually suspected when on standard chest radiographs or CT scans a lesion is detected in the characteristic location for a sequestration, in the appropriate clinical setting. CT scans, however, do not reliably define the vascular anatomy. An arteriogram has been considered vital in documenting the systemic blood supply, allowing definitive diagnosis as well as preoperative planning.
However, the advent of new noninvasive imaging techniques has changed this thinking. Multislice CT scanning reveals not only the radiographic features of the sequestration but also its complex character. In addition, multislice CT helps identify the aberrant arterial supply and venous drainage of the sequestration.6-8
Magnetic resonance angiography allows the delineation of the systemic arterial supply and the precise localization, orientation, and even tissue composition of the sequestration.7-9 Ultrasonography with color Doppler and triplex Doppler also is useful in documenting vascular anatomy.7
Management of an asymptomatic pulmonary sequestration with no connection to the surrounding lung is controversial; however, most references advocate resection of the lesions because of the likelihood of recurrent lung infection, the need for larger resection if the sequestration becomes chronically infected, and the possibility of hemorrhage from arteriovenous anastomoses.10 Surgical resection is the treatment of choice for patients who present with infection or symptoms resulting from compression of normal lung tissue. Intralobar lesions often require lobectomy because the margins of the sequestration may not be clearly defined.
Conclusion
Intralobar sequestration is a rare condition that may present as recurrent pneumonia or an asymptomatic left lower lobe mass on a chest radiograph. Intralobar sequestrations are almost always located in the posterior basilar segment of the left lower lobe. The definitive diagnosis needs to be established preoperatively-and the vascular supply delineated-to avoid potentially life-threatening hemorrhage. Magnetic resonance angiography may replace standard angiography as a noninvasive method of defining the vascular anatomy. Surgical resection is curative for symptomatic patients
References:
REFERENCES
1.
Pryce DM. Lower accessory pulmonary artery with intralobular sequestration of lung: a report of seven cases.
J Pathol.
1946;58:457-467.
2.
Savic B, Birtel FJ, Tholen W, et al. Lung sequestration: report of seven cases and review of 540 published cases.
Thorax.
1979;34:96-101.
3.
Fraser RS, Colman N, Muller NL, et al. Developmental anomalies affecting the airways and lung parenchyma. In: Fraser RS, Colman N, Muller NL, et al, eds.
Fraser and Pare's Diagnosis of Diseases of the Chest.
4th ed. Philadelphia: WB Saunders Co; 1999:597-635.
4.
Hofman FN, Pasker HG, Speekenbrink RG. Hemoptysis and massive hemothorax as presentation of intralobar sequestration.
Ann Thorac Surg.
2005;80:2343-2344.
5.
Silverman ME, White CS, Ziskind AA. Pulmonary sequestration receiving arterial supply from the left circumflex coronary artery.
Chest.
1994;106:948-949.
6.
Ahmed M, Jacobi V, Vogl TJ. Multislice CT and CT angiography for non-invasive evaluation of bronchopulmonary sequestration.
Eur Radiol.
 2004;14:2141-2143.
7.
 Ko SF, Ng SH, Lee TY, et al. Noninvasive imaging of bronchopulmonary sequestration.
AJR.
2000;175:1005-1012.
8.
Felker RE, Tonkin IL. Imaging of pulmonarysequestration.
AJR.
1990;154:241-249.
9.
Ko SC, Chang YC, Liaw YS, et al. Diagnosis of pulmonary sequestration by magnetic resonanceimaging.
J Formos Med Assoc.
1998;97:220-223.
10.
Van Raemdonck D, De Boeck K, Devlieger H, et al. Pulmonary sequestration: a comparison between pediatric and adult patients.
Eur J Cardiothorac Surg.
2001;19:388-395.
