- Clinical Technology
- Adult Immunization
- Hepatology
- Pediatric Immunization
- Screening
- Psychiatry
- Allergy
- Women's Health
- Cardiology
- Pediatrics
- Dermatology
- Endocrinology
- Pain Management
- Gastroenterology
- Infectious Disease
- Obesity Medicine
- Rheumatology
- Nephrology
- Neurology
- Pulmonology
Mites and HTLV-1 at the Crux of a 10-Year Itch and Plaque-Like Lesions
Immunosuppression that is associated with human T-cell lymphotropic virus 1 (HTLV-1) infection predisposes to hyperinfective strongyloidiasis.1,2
Key words: Crusted scabies, Human T-cell lymphotropic virus 1, Adult T-cell leukemia/lymphoma
Immunosuppression that is associated with human T-cell lymphotropic virus 1 (HTLV-1) infection predisposes to hyperinfective strongyloidiasis.1,2 One study suggests that it also predisposes to crusted scabies.3 In a study of Australian aborigines by Mollison and colleagues,4 all 5 cases of crusted scabies were in patients who were seropositive for HTLV-1. In a series by Blas and colleagues3 conducted in Peru, 16 of 23 patients (69.6%) with crusted scabies were HTLV-1–positive.
We present a case of crusted scabies that persisted for 10 years before diagnosis. HTLV-1 infection was the underlying disease, although the erroneous application of topical corticosteroids may have contributed to the severity of the lesions. Acute adult T-cell leukemia/lymphoma (ATLL) later developed as a consequence of HTLV-1 seropositivity.
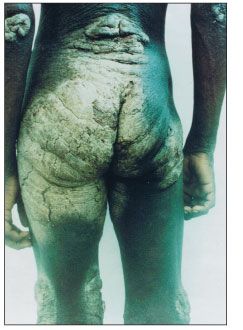
Figure 1 –Extensive hyperkeratotic, cream-colored plaques with deep fissures are seen over the buttocks, lower back, knees, elbows, and axillary folds in this patient in whom crusted scabies and human T-cell lymphotropic virus 1 infection was diagnosed.
Case report
A 17-year-old West Indian patient was seen at Princess Margaret Hospital in the Commonwealth of Dominica. He presented with extensive hyperkeratotic, cream-colored plaques with deep fissures over the buttocks, lower back, knees, elbows, and axillary folds (Figure 1). He reported that these symptoms had persisted for 4 years. The scalp and nails were spared.
Severe pruritus and a generalized papular rash that began to emerge when the patient was 7 years old preceded manifestation of the lesions. A misdiagnosis of atopic dermatitis was made at that time, and the patient received recurrent treatment with 1% hydrocortisone cream. As the pruritus gradually subsided, plaques progressively developed. The patient experienced social and familial rejection because of the skin lesions and subsequently lived in public pavilions. He was not sexually active, never used illicit intravenous drugs, and had no history of blood transfusion.
Other elements of his physical examination were normal. Skin biopsy samples showed numerous deep scabetic mites. The white blood cell (WBC) count was 11,000/µL, with 42% eosinophils, 32% lymphocytes, 21% neutrophils, and 5% monocytes. The absolute lymphocyte count was 3800/µL, and no atypical lymphocytes were detected on blood film. His hemoglobin level was 13.0/µL, platelet count was 292 × 103/µL, and erythrocyte sedimentation rate was 19 mm/h. Serum electrolyte, uric acid, calcium, blood glucose, total protein and albumin, and hepatic enzyme levels were normal.
Enzyme-linked immunosorbent assay with confirmation by Western blot testing showed negative results for serum antibody to HIV but positive results for HTLV-1. A diagnosis of crusted scabies and HTLV-1 infection was made.
The patient received inpatient treatment in an isolation room. The hyperkeratotic lesions were initially treated with a keratolytic ointment consisting of sulfur and 25% salicylic acid ointment and then with a formulation consisting of sulfur and 10% salicylic acid ointment for 7 days before being treated with 5% permethrin cream. The cream was applied to the entire body for 12 hours. The application was repeated after 72 hours.

Figure 2 –The lesions resolved after treatment with a keratolytic ointment containing sulfur and salicylic acid and 5% permethrin cream.
The patient’s skin lesions resolved after 1 month of treatment (Figure 2). A skin biopsy specimen was negative for the presence of mites. No cross infection to other patients or staff occurred. Neither was there disease recurrence during the 6 months of follow-up.
Nine months after receiving treatment for scabies, the patient presented with oropharyngeal candidiasis, right lobar pneumonia, generalized lymphadenopathy, generalized papular rashes, hepatosplenomegaly, and a WBC count of 84,300/µL with atypical lymphocytosis. A diagnosis of acute ATLL was made. The patient died within 48 hours of hospital admission. Autopsy findings showed that the cause of death was mediastinal lymph node abscess with Escherichia coli septicemia.
Discussion
Scabies is caused by the mite Sarcoptes scabiei var hominis, an ectoparasite with a worldwide distribution. In its mildest presentation, it causes pruritus, especially at night, in the interdigital and genital areas, lower abdomen, axillary folds, and buttocks. The most severe form, crusted scabies, also called Norwegian scabies, presents with marked crusting and hyperkeratosis and can mimic dermatoses such as psoriasis, Darier disease, or seborrheic dermatitis. Misdiagnosis is common.
This rare, fulminant, and highly contagious variant was initially described in patients with leprosy by Danielson and Boeck in 1848.5 Other cases were later described in association with immunosuppression from disorders such as malnutrition, chronic alcoholism, diabetes mellitus, lymphoreticular malignancies, Down syndrome and other causes of mental retardation, HIV/AIDS, and HTLV-1 infection; therapy such as with corticosteroids or with blood or organ transplant; poor hygiene; or overcrowding.3,4,6,7
Our patient’s age at presentation with ATLL may suggest mother-to-child transmission of HTLV-1; leukemogenesis takes about 20 to 40 years to develop.8 Some authors have suggested that crusted scabies may be an indicator of later development of ATLL in HTLV-1–infected patients,9 as seen in this case.
The exact mechanism through which HTLV-1 predisposes to crusted scabies is not known; however, immunological changes seen in patients with crusted scabies include a very high eosinophil count and elevated IgG, IgA, IgE, and interleukin-4 levels.10
Our patient responded well to combination therapy with keratolytic ointment and 5% permethrin cream. Oral ivermectin at a dose of 200 µg/kg is an alternative treatment for severe scabies.11,12 No effective intervention is available for HTLV-1 infection; treatment focuses on management of associated diseases that may emerge, such as lymphomas, leukemias, and neurological disorders. As commonly occurs in patients who have HTLV-1–associated ATLL, the cause of death in our patient was attributed to infectious complications.
HTLV-1 is endemic to the Caribbean, parts of South and Central America, Japan, Melanesia, and sub-Saharan Africa. HTLV-1 is transmitted in a way similar to that of HIV. The incidence of infection is low in the United States; high-risk populations include immigrants from areas where HTLV-1 is endemic, children or sex partners of immigrants from areas of endemicity, sex workers, persons who have many sex partners and do not adhere to safe sex practices, injection drug users, and persons who receive blood transfusions from blood banks that do not adhere to blood screening protocols.
Crusted scabies was a predictor of HTLV-1 infection in our patient, who was from an area of endemicity-the West Indies. The findings are similar to those observed by Mollison and colleagues4 in Australian aborigines and by Blas and colleagues3 in Peru. We have also treated 2 other patients with crusted scabies. Both were HTLV–1–positive and had no other underlying disease. Like other authors, we suggest that crusted scabies is a clinical marker of HTLV-1 infection. Patients should be closely monitored for subsequent development of ATLL.
References:
REFERENCES
1. Adedayo O, Grell G, Bellot P. Hyperinfective strongyloidiasis in the medical ward: review of 27 cases in 5 years. South Med J. 2002;95:711-716.
2. Gotuzzo E, Terashima A, Alvarez H, et al. Strongyloides stercoralis hyperinfection associated with human T cell lymphotropic virus type-1 infection in Peru. Am J Trop Med Hyg. 1999;60:146-149.
3. Blas M, Bravo F, Castillo W, et al. Norwegian scabies in Peru: the impact of human T cell lymphotropic virus type 1 infection. Am J Trop Med Hyg. 2005;72:855-857.
4. Mollison LC, Lo ST, Marning G. HTLV-I and scabies in Australian aborigines. Lancet. 1993;341:1281-1282.
5. Parish LC, Lomholt G. Crusted scabies: alias Norwegian scabies. Int J Dermatol. 1976;15:747-748.
6. Bergman JN, Dodd WA, Trotter MJ, et al. Crusted scabies in association with human T-cell lymphotropic virus 1. J Cutan Med Surg. 1999;3:148-152.
7. Daisley H, Charles W, Suite M. Crusted (Norwegian) scabies as a pre-diagnostic indicator for HTLV-1 infection. Trans R Soc Trop Med Hyg. 1993;87:295.
8. Murphy EL, Hanchard B, Figueroa JP, et al. Modelling the risk of adult T-cell leukemia/lymphoma in persons infected with human T-lymphotropic virus type 1. Int J Cancer. 1989;43:250-253.
9. del Giudice P, Sainte Marie D, Gérard Y, et al. Is crusted (Norwegian) scabies a marker of adult T cell leukemia/lymphoma in human T lymphotropic virus type 1-seropositive patients? J Infect Dis. 1997;176:1090-1092.
10. Roberts LJ, Huffam SE, Walton SF, Currie BJ. Crusted scabies: clinical and immunological findings in seventy-eight patients and a review of the literature. J Infect. 2005;50:375-381.
11. Cordoliani F, Vasseur E, Baccard M, et al. Ivermectin-responsive crusted scabies in HTLV1 carrier. Dermatology. 1996;192:351-352.
12. Fawcett RS. Ivermectin use in scabies. Am Fam Physician. 2003;68:1089-1092.
