- Clinical Technology
- Adult Immunization
- Hepatology
- Pediatric Immunization
- Screening
- Psychiatry
- Allergy
- Women's Health
- Cardiology
- Pediatrics
- Dermatology
- Endocrinology
- Pain Management
- Gastroenterology
- Infectious Disease
- Obesity Medicine
- Rheumatology
- Nephrology
- Neurology
- Pulmonology
Chylothorax: A review of current management strategies
ABSTRACT: The most common causes of chylothorax are neoplasm-particularly lymphoma-and trauma. The usual presentingsymptom is dyspnea resulting from the accumulationof pleural fluid. The diagnosis of chylothorax is established bymeasuring triglyceride levels in the pleural fluid; a triglyceridelevel of greater than 110 mg/dL supports the diagnosis. The initialapproach to management involves chest tube drainage ofthe pleural space. The administration of medium-chain triglyceridesas a source of fat is often useful. If drainage remains unchanged,parenteral alimentation should be started. Surgicalintervention is indicated if conservative management is notsuccessful or if nutritional deterioration is imminent. If chylothoraxpersists after ligation of the thoracic duct, options mayinclude percutaneous embolization, pleuroperitoneal shunt,and pleurodesis. (J Respir Dis. 2008;29(8):325-333)
ABSTRACT:The most common causes of chylothorax are neoplasm-particularly lymphoma-and trauma. The usual presenting symptom is dyspnea resulting from the accumulation of pleural fluid. The diagnosis of chylothorax is established by measuring triglyceride levels in the pleural fluid; a triglyceride level of greater than 110 mg/dL supports the diagnosis. The initial approach to management involves chest tube drainage of the pleural space. The administration of medium-chain triglycerides as a source of fat is often useful. If drainage remains unchanged, parenteral alimentation should be started. Surgical intervention is indicated if conservative management is not successful or if nutritional deterioration is imminent. If chylothorax persists after ligation of the thoracic duct, options may include percutaneous embolization, pleuroperitoneal shunt, and pleurodesis. (J Respir Dis. 2008;29(8):325-333)
Chyle in the pleural space was first described by Bartolet in 1633, and since that time, numerous causes have been well described.1 The pleural fluid in chylothorax consists of chylomicrons and very-low-density lipoproteins. It results from an anatomical disruption of the thoracic duct or a major lymphatic contributory or both.
In 1948, Lampson2 reported the first successful treatment of chylothorax by supradiaphragmatic ligation of the thoracic duct. Although chylothorax accounts for a small proportion of pleural effusions, prompt recognition is needed to avoid malnutrition and to prevent immunodeficiency.
In this article, we will review the various causes of chylothorax, the diagnostic workup, and management options.
ANATOMY
Chyle passes from the intestinal lymphatics to the cisterna chyli and through the thoracic duct to empty into the venous system. The thoracic duct begins at the cisterna chyli near the T12 vertebra and ascends through the aortic hiatus of the diaphragm on the anterior surface of the vertebral body between the aorta and azygos vein into the posterior mediastinum.
At the level of the T5 vertebra, the duct crosses to the left of the vertebral column and ascends behind the aortic arch to the left of the subclavian artery adjacent to the mediastinal pleura.
At the level of the transverse process of the C7 vertebra, the thoracic duct turns laterally and runs anterior to the vertebral and thyrocervical arteries and the sympathetic trunk. Passing behind the carotid sheath, the duct descends anterior to the origin of the left subclavian artery and terminates near the junction of the internal jugular and subclavian veins.
A bicuspid valve at the lymphovenous junction prevents the reflux of blood into the duct. The duct has numerous valves throughout its length. However, in up to 50% of persons, the route of the thoracic duct is anomalous and unpredictable, making it more susceptible to damage during surgical procedures. 3 This duct carries lymph from the entire body except from the right side of the head, neck, and chest; both lungs; and the right upper extremity. The lymph from the right side of the neck and chest then empties into the right lymphatic duct.
Extensive anastomotic vessels are between various lymphatics, and numerous lymphaticovenous anastomoses are between the thoracic duct and the azygos, intercostal, and lumbar veins.4 The richness of this collateral circulation allows the safe ligation of the thoracic duct at any level.
PHYSIOLOGY
The word "chyle" comes from the Latin word meaning "juice" and is applied to lymph of intestinal origin. Ingested fats are transported by chyle into the venous blood via the thoracic duct. In the fasting state, chyle is usually clear because of its low fat content; the protein content and volume are also diminished. After ingestion of a fatty meal, chyle assumes its characteristic milky appearance. It is estimated that up to 60% of ingested fat passes into the lymphatics.
Normally, 1500 to 2500 mL of chyle is emptied into the venous system daily. The protein content of chyle is more than 3 g/dL, and the electrolyte composition is similar to that of serum.5 The chyle formed in the cisterna chyli is an odorless, white, opaque liquid. Analysis of chyle reveals a white blood cell count of 2000 to 10,000/µL, with approximately 90% lymphocytes, which generally renders this fluid bacteriostatic. It is believed that most of the lymphocytes in chyle are T lymphocytes.6
Chemical analysis reveals protein and fat globules that stain with Sudan III dyes. Chyle is alkaline and has a specific gravity of greater than 1.012; it will settle on standing with a fat-rich portion on the top and cellular sediment on the bottom. Chyle is high in neutral fats and fatty acids but low in cholesterol.
Flow through the thoracic duct can vary widely-from as low as 14 mL/h in the fasting state to over 100 mL/h postprandial. Thoracic duct flow is related to the duct wall smooth muscle response to splanchnic and vagal stimulation. Serotonin, norepinephrine, histamine, dopamine, and acetylcholine all increase thoracic duct contraction and chyle flow.7 In addition to fasting, opiate administration will decrease the volume of chyle production.
PATHOGENESIS
The pathogenesis of chylothorax can be divided into 2 major categories: medical causes and trauma. Chylothorax from medical causes results from either extrinsic compression or infiltration of the thoracic duct, which causes an increase in intraductal pressure. This increased pressure promotes the formation of dilated collateral channels that eventually drain into the pleural space.
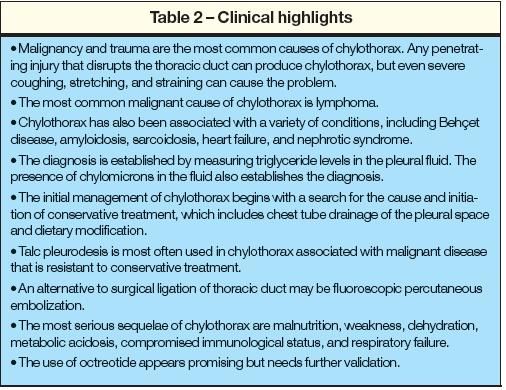
The most common cause of chylothorax is neoplasm, which is responsible for more than 50% of cases (Table 1). The most common malignancy leading to this condition is lymphoma,8 which leads to chylothorax by compressing or invading the thoracic duct or obliterating the lymphatics after radiation therapy.9 Obstruction of the thoracic duct by lymphoma or bronchogenic carcinoma tends to cause a right-sided chylothorax when the lower portion of the duct is involved and a left-sided chylothorax when the upper portion of the thoracic duct is involved. Chylothorax that occurs in the setting of malignancy below the diaphragm invariably indicates metastasis.10
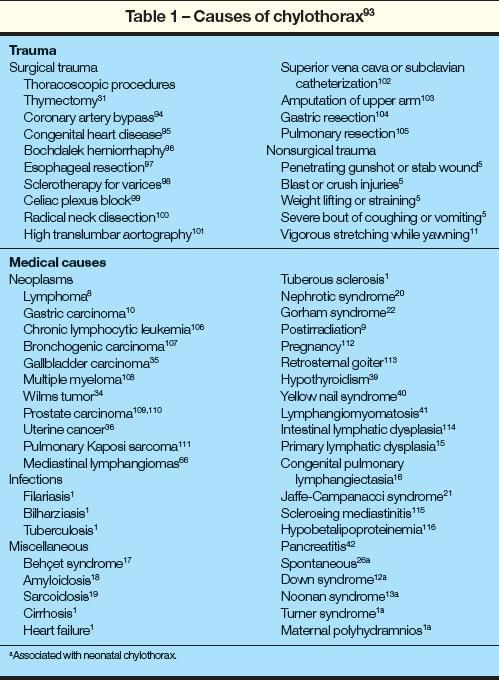
The other leading cause of chylothorax is trauma, which can be further categorized as surgical and nonsurgical trauma. Any penetrating injury that disrupts the thoracic duct can produce chylothorax, but even severe coughing, stretching, and straining have been reported to cause chylothorax.11 Surgical procedures on the heart or mediastinum, operations involving the neck such as radical neck dissections, and placement of catheters in the superior vena cava for hemodynamic monitoring can also cause chylothorax.
Chylothorax is the most common cause of pleural effusion in neonates, and it usually appears spontaneously.1,12-16 Systemic conditions such as Behet syndrome,17 amyloidosis, 18 sarcoidosis,19 heart failure, and nephrotic syndrome20 also are associated with chylothorax. Jaffe-Campanacci syndrome, which includes disseminated nonossifying fibromata, has also been linked with chylothorax.21
Chylothorax develops in up to 17% of patients with Gorham syndrome, which is a rare disease associated with progressive osteolysis and intraosseous angiomatosis of lymphatics and blood vessels.22 Pulmonary lymphangiomyomatosis is characterized by the proliferation of immature smooth muscle throughout the peribronchial, perivascular, and perilymphatic region; the perilymphatic proliferation of smooth muscle results in lymphatic obstruction and chylothorax in up to 50% of patients.23 This condition may occur as a part of the pulmonary tuberous sclerosis syndrome.
Chylothorax that develops acutely without an underlying cause is referred to as spontaneous chylothorax. 24,25 When the cause of chylothorax is still not established after a detailed workup and history, it may be considered to be spontaneous chylothorax.
A sudden increase in duct pressure from coughing, especially after a heavy meal when the duct is engorged, may be a rare and overlooked cause.26,27
Most cases of chylothorax are unilateral, but bilateral chylothorax has also been reported.25,26,28-33 Kaposi sarcoma, for example, has been reported to result in bilateral chylothorax.33
Chylothorax and chyloperitoneum have been reported in patients with nephritic syndrome20; malignancies such as Wilms tumor, 34 gallbladder carcinoma,35 uterine cancer,36 gastric carcinoma, 10 and lymphoma37; retroperitoneal surgery38; hypothyroidism39; sarcoidosis19; yellow nail syndrome40; primary lymphatic dysplasia15; lymphangiomyomatosis41; and pancreatitis.42 In addition, the occurrence of chylothorax and chyloperitoneum has been classified as idiopathic.43
CLINICAL FEATURES AND DIAGNOSIS
The usual presenting symptom of chylothorax is dyspnea resulting from accumulation of pleural fluid.8 Chest pain and fever are uncommon because chyle is not irritating to the pleural surface. Traumatic chylothorax usually develops within 2 to 10 days postinjury.5 In medical causes of chylothorax, the onset of symptoms is more insidious. Rarely, spontaneous chylothorax may present as a sudden neck mass.24,31 The severity of symptoms is related to the rate of accumulation of chyle and the size of the pleural effusion.
The most serious sequelae of chylothorax are malnutrition, weakness, dehydration, metabolic acidosis, respiratory failure, and compromised immunological status as a result of the loss of chyle, which is rich in proteins, fats, electrolytes, bicarbonate, lymphocytes, and fat-soluble vitamins. In some cases, prolonged chylothorax may be associated with reversible T-cell deficiency. 44 Hypoalbuminemia and lymphopenia secondary to prolonged loss of chyle increase the risk of systemic bacterial and viral infections. There is a good correlation between rate of chyle loss, operative intervention, and survival.45
Chyle is often suspected only after thoracentesis. Chyle is distinctively white, odorless, and milky in appearance. The diagnosis of chylothorax is established by measuring triglyceride levels in the pleural fluid. If the triglyceride level is greater than 110 mg/dL, a diagnosis of chylothorax is likely; if the level is less than 50 mg/dL, chylothorax is unlikely. When levels are 50 to 110 mg/dL, lipoprotein analysis should be performed. Chylomicrons in the fluid establish the diagnosis of chylothorax.46
Milky or creamy pleural fluid also can be associated with pseudochylothorax, which may occur in patients with chronic diseases such as tuberculosis.5 The turbidity in this condition is the result of high levels of cholesterol or lecithin-globulin complexes rather than chylomicrons in chylothorax. Pseudochylothorax effusions are usually of long-standing duration and may cause thickened and even calcified pleura.
The presence of cholesterol crystals in the fluid is diagnostic of pseudochylothorax; chylomicrons are never present on lipoprotein analysis. Both chylous and pseudochylous fluid remains opaque after centrifugation. Since pseudochylothorax is associated with cholesterol levels of greater than 250 mg/dL and triglyceride levels of less than 110 mg/dL, the turbidity that is caused by the high cholesterol level will clear with the addition of 2 mL of ethyl ether. Thus, whenever there is any doubt, the fluid should be analyzed for chylomicrons.
Another useful test is the ingestion of lipophilic dye or radiolabeled triglyceride (131I-triolein). The presence of the dye color in the fluid within 1 hour or detection of high radioactivity in the pleural fluid after 48 hours confirms the presence of chylothorax.5 Lymphangiography may help define the site of chyle leak or obstruction or penetrating trauma in spontaneous chylothorax and in lymphangiomatous malformations. 47 It has also demonstrated a therapeutic role in assisting occlusion of the postoperatively damaged lymphatic vessel. Occlusion may occur from an inflammatory granulomatous reaction by the contrast dye during extravasation.48
MANAGEMENT
The initial management of chylothorax begins with the determination of the cause. Surgical causes are generally more obvious than medical causes. Because lymphoma is the most common nonsurgical cause of chylothorax, a CT scan of the chest and abdomen should be performed to evaluate the mediastinal and paraaortic lymph nodes.
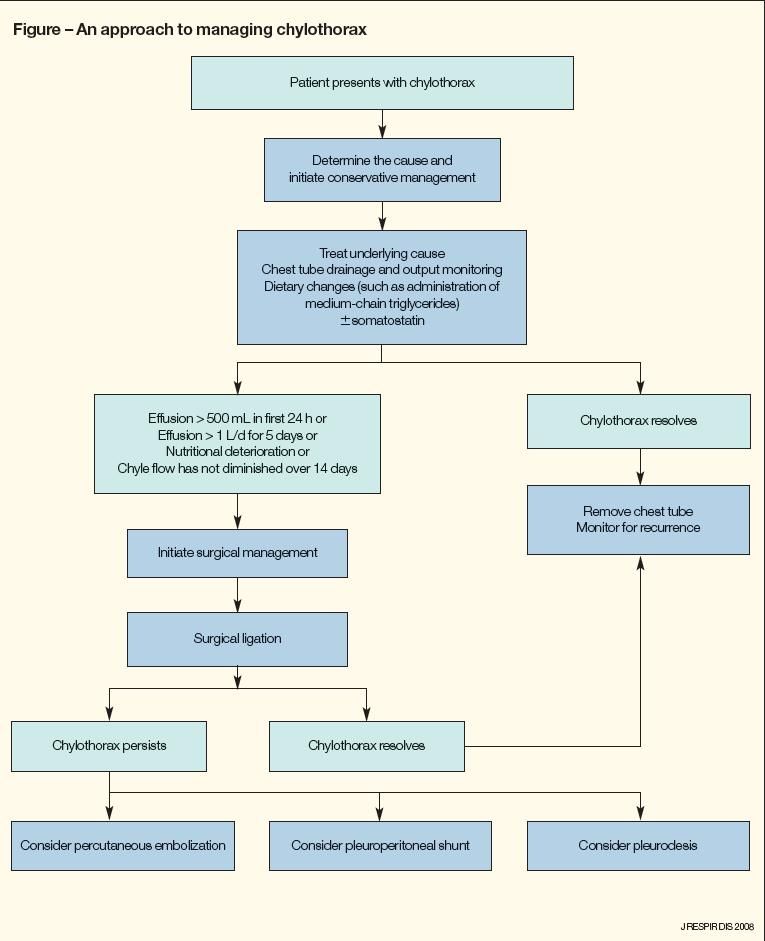
Primary treatment must be directed at the underlying cause. In most instances, surgery should be pursued only after failure of conservative therapy (Figure). However, the timing of surgical management is unclear.
Conservative therapy
While determining the cause of chylothorax, the initial approach to management involves chest tube drainage of the pleural space.49-51 Continuous suction drainage helps relieve the pressure of chyle on the lungs, reexpands the partially collapsed lungs, obliterates the pleural space, and permits an a
ccurate measurement of chyle production. Lung reexpansion is sometimes hindered by the formation of a fibrinous membrane around the lung, which may necessitate surgical intervention.52
The rate of chyle leakage can be measured and recorded if the chest tube is in place. Chest tube drainage of less than 500 mL during the first 24 hours after complete oral intake cessation and total parenteral nutrition (TPN) may predict successful conservative treatment.53
Because up to 3 L of chyle may drain daily, large amounts of fluid, electrolytes, fat, protein, and lymphocytes may be lost. Careful monitoring of chyle output and replacement of daily losses are essential in addition to monitoring the patient's weight; serum albumin, total protein, and electrolyte levels; and absolute lymphocyte count. A nonfat, high-protein, high-calorie diet will produce some reduction of chyle flow.
Administration of medium-chain triglycerides as a source of fat is invaluable. 51 Medium-chain triglycerides are absorbed directly into the portal system rather than the intestinal and thoracic lymphatics. With the use of medium-chain triglycerides, not only is the nutrition satisfactorily maintained but also thoracic duct flow is minimized to promote healing of the leak.
It has been suggested that trioctanoin (C8:0) may be the preferred medium-chain triglyceride substrate for patients with chylothorax. 54,55 Medium-chain triglyceride diets have met with variable success in the treatment of chylothorax because any oral/enteral feeding increases lymph flow56 and because intestinal triglycerides are derived from both endogenous and exogenous sources.57
If drainage remains unchanged, parenteral alimentation should be started. Others have recommended stopping oral feeding and initiating TPN at the time of diagnosis.5 Comparison of enteral versus parenteral nutrition in the setting of chylothorax shows that thoracic duct closure occurs faster with TPN.58
Etilefrine is an α- and β-adrenergic sympathomimetic drug used in postural hypotension. It has also been used in limited cases for chlylothorax as an adjunct to conservative therapy.59,60 The benefit of etilefrine may be attributed to smooth muscle contraction of the thoracic duct. Consideration of etilefrine's benefits should be individualized because of this agent's other sympathetic effects.
If nutritional deterioration is imminent, surgical intervention is indicated. If the patient is receiving mechanical ventilation, adding positive end-expiratory pressure may lead to an increase in intrathoracic pressure, resulting in approximation of the 2 intrapleural surfaces and potentially decreasing chyle leakage.61 Thomson and Simms62 reported successful reinfusion of chyle drained from a chest tube using blood filters and a volumetric pump, but anaphylactic reactions have been reported after intravenous transfusion of chyle.63
Somatostatin is an inhibitor of gastric, pancreatic, and intestinal secretions, thereby helping to keep the GI tract empty, which, in turn, decreases the chyle production.64 Octreotide is an analog of somatostatin that has been used in conjunction with other modalities (TPN, effusion drainage) in conservative management of chylothorax of various causes.65-67 Because of its longer half-life, octreotide offers a subcutaneous as well as an intravenous route of administration.
The support for octreotide is limited to case reports and small series, making its therapeutic effectiveness difficult to differentiate from spontaneous improvement or other concurrent treatments. Because of the lack of evidence, we cannot recommend octreotide as a first-line agent at this time. Although this form of intervention appears to be similar to somatostatin, the use of octreotide needs further validation in clinical trials.
Treatment of the underlying cause may be especially helpful in patients with chylothorax secondary to lymphoma, when radiotherapy is directed at the mediastinum to resolve the tumor mass. Mediastinal tumors associated with chylothorax, such as lymphangiomas, also respond to radiotherapy.68
The duration of conservative management is not firmly established and depends on pathogenesis, underlying comorbid illness, and institutional experience. Operative intervention for chylothorax should be considered when more than 500 mL of chyle drains in the first 24 hours despite fasting and TPN, average loss has exceeded 1 L per day for 5 days in adults, chyle flow has not diminished in 14 days, or nutritional complications appear imminent (Table 2).52,69
Surgical therapy
Two weeks is often used as the limit for resolution by conservative management, but no large controlled studies have confirmed this.45,52 Patients with drainage of more than 1 L/d may benefit from earlier (5 to 7 days) surgical intervention because of a higher mortality with increased output.69
Failure of conservative treatment in cases of surgical chylothorax requires surgical intervention for definitive management. As noted above, Lampson2 first demonstrated that chylothorax could be controlled by ligation of the thoracic duct. Preoperative administration of lipophilic dye (such as Evans blue) or cream helps locate the site of lymphatic leakage during the procedure. The thoracic duct is then identified, isolated, and ligated just above the aortic hiatus between T8 and T12.70 After ligation, there is usually some obstruction to lymph flow distal to the ligated site until new collateral channels are formed (2 to 3 weeks).71
An abdominal approach to ligate the thoracic duct is an alternative when a thoracic approach is not feasible72; others have described a posterior extrapleural approach to ligation of the thoracic duct.73 Video-assisted thoracic surgery has provided an effective and potentially less invasive approach to managing chylothorax.74,75 Successful ligation of the thoracic duct by thoracoscopy using fibrin glue or endoscopic clips at the site of the leak has been attempted and has the advantages of less postoperative pain and a shorter hospital stay.76-78 Graham and colleagues74 described successful use of video-assisted thoracic surgery in 10 patients with chylothorax and recommended early intervention with this procedure.
Early thoracoscopic repair has 2 major advantages: the risk of malnutrition is minimized and postthoracotomy pain and discomfort are avoided. When it is impossible to identify the duct surgically, especially in malignancy and radiation fibrosis, pleurodesis or pleurectomy may be used.79 These procedures have been used alone and in combination with thoracotomy and ligation of the thoracic duct.
Talc pleurodesis is most often used in chylothorax associated with malignant disease that is resistant to conservative treatment.79 Other approaches include intrapleural infusion of tetracycline,80 fibrin glue,81 and OK 43282 (a Su strain of Streptococcus pyogenes). Intrapleural bleomycin has been found to be effective in patients with chylothorax secondary to lymphoma.83
The surgical approach to managing nontraumatic chylous effusions is more variable. Milsom and coworkers84 recommend pleuroperitoneal shunting after failure of conservative therapy and before thoracotomy. Murphy and associates85 recommend placing a shunt if the drainage persists beyond 5 days. A pleuroperitoneal shunt consists of pleural and peritoneal catheters connected to a manual pumping chamber capable of handling viscous fluid such as chyle. The system contains a one-way valve that allows drainage from pleura to the peritoneal cavity where the fluid is absorbed.86
Shunting seems to prevent further loss of chyle and its nutritionally important constituents,85 potentially reducing the need for TPN.87 The fluid in the peritoneal cavity is absorbed by the lymphatic vessels, mainly those of the diaphragm on the right side overlying the liver, which, in turn, drain into the right thoracic duct. Occlusion of the shunt with fibrinous debris occurs in about 10% of patients and requires replacement.88 Obviously, concomitant presence of ascites is a contraindication to pleuroperitoneal shunt placement, and a pleurovenous shunt may be considered in these cases.89
An alternative to surgical ligation of thoracic duct may be fluoroscopic percutaneous embolization. This minimally invasive procedure requires pedal lymphography to access the lymphatic duct via transabdominal puncture.90-92 Once access is obtained, a small catheter (3 to 4 F) using contrast dye opacifies the thoracic duct and collateral branches. The use of various coils or glue or both can occlude the thoracic duct.
Percutaneous embolization offers a minimally invasive procedure with low morbidity, and it can be safely performed earlier than surgery even in debilitated patients.92 Limitations of this procedure include difficulties in gaining access to the lymphatic duct and pedal lymphography. The success rate is variable, ranging from 45% to 100%.91,92
CONCLUSIONS
There are numerous causes of chylothorax.93 The cause should be ascertained because treatment will be tailored accordingly. Other considerations include nutritional status, severity of the underlying disease, and proper delineation of the thoracic duct anatomy in the planning of the treatment. When conservative management fails, appropriate surgical intervention or percutaneousembolization must be considered.
References:
REFERENCES
1. Light RW. Chylothorax and pseudochylothorax. In: Light RW, ed. Pleural Diseases. 4th ed. Baltimore: Williams & Wilkins; 1995:284-298.
2. Lampson RS. Traumatic chylothorax. A review of literature and report of a case treated by mediastinal ligation of the thoracic duct. J Thorac Surg. 1948;17:778-791.
3. Kausel HW, Reeve TS, Stein AA, et al. Anatomic and pathologic studies of the thoracic duct. J Thorac Surg. 1957;34:631-641.
4. Hesseling PB, Hoffman H. Chylothorax. A review of the literature and report of 3 cases. S Afr Med J. 1981;60:675-678.
5. Sassoon CS, Light RW. Chylothorax and pseudochylothorax. Clin Chest Med. 1985;6:163-171.
6. Machleder HI, Paulus H. Clinical and immunological alterations observed in patients undergoing long-term thoracic duct drainage. Surgery. 1978;84:157-165.
7. Ferguson MK, Shahinian HK, Michelassi F. Lymphatic smooth muscle responses to leukotrienes, histamine, and platelet activating factor. J Surg Res. 1988;44:172-177.
8. Doerr CH, Allen MS, Nichols FC 3rd, Ryu JH. Etiology of chylothorax in 203 patients. Mayo Clin Proc. 2005;80:867-870.
9. Strausser JL, Flye MW. Management of nontraumatic chylothorax. Ann Thorac Surg. 1981;31:520-526.
10. Majoor CJ, Aliredjo RP, Dekhuijzen PN, et al. A rare cause of chylothorax and lymph edema. J Thorac Oncol. 2007;2:247-248.
11. Reilly KM, Tsou E. Bilateral chylothorax. A case report following episodes of stretching. JAMA. 1975;233:536-537.
12. Ho NK, Leong NK, Lim SB. Chylothorax in Down's syndrome associated with hydrops fetalis. J Singapore Paediatr Soc. 1989;31:90-92.
13. Chan DK, Ho NK. Noonan syndrome with spontaneous chylothorax at birth. Aust Paediatr J. 1989;25:296-298.
14. Pauwels R, Oomen C, Huybrechts W, van der Straeten M. Chylothorax in adult age in association with congenital lymphedema. Eur J Respir Dis. 1986;69:285-287.
15. Smeltzer DM, Stickler GB, Fleming RE. Primary lymphatic dysplasia in children: chylothorax, chylous ascites, and generalized lymphatic dysplasia. Eur J Pediatr. 1986;145:286-292.
16. Moerman P, Vandenberghe K, Devlieger H, et al. Congenital pulmonary lymphangiectasis with chylothorax: a heterogenous lymphatic vessel abnormality. Am J Med Genet. 1993;47:54-58.
17. Konishi T, Takeuchi H, Iwata J, Nakano T. Behçet's disease with chylothorax-case report. Angiology. 1988;39(1, pt 1):68-71.
18. Fairfax AJ, McNabb WR, Spiro SG. Chylothorax: a review of 18 cases. Thorax. 1986;41:880-885.
19. Cappell MS, Friedman D, Mikhail N. Chyloperitoneum associated with chronic severe sarcoidosis. Am J Gastroenterol. 1993;88:99-101.
20. Moss R, Hinds S, Fedullo AJ. Chylothorax: a complication of the nephrotic syndrome. Am Rev Respir Dis. 1989;140:1436-1437.
21. Kotzot D, Stoss H, Wagner H, Ulmer R. Jaffe Campanacci syndrome: case report and review of literature. Clin Dysmorophol. 1994;3:328-334.
22. Tie ML, Poland GA, Rosenow EC 3rd. Chylothorax in Gorham's syndrome. A common complication of a rare disease. Chest. 1994;105:208-213.
23. Hughes E, Hodder RV. Pulmonary lymphangiomyomatosis complicating pregnancy. A case report. J Reprod Med. 1987;32:553-557.
24. Pantin CF, Emerson PA. Recurrent supraclavicular chylous collection and chylothorax. Respir Med. 1989;83:445-446.
25. Garcia Restoy E, Bella Cueto F, Espejo Arenas E, Aloy Duch A. Spontaneous bilateral chylothorax: uniform features of a rare condition. Eur Respir J. 1988;1:872-873.
26. Dhand R, Jolly N, Bambery P, Deodhar SD. Bilateral spontaneous chylothorax. Indian J Chest Dis Allied Sci. 1988;30:51-55.
27. Paes ML, Powell H. Chylothorax: an update. Br J Hosp Med. 1994;51:482-490.
28. Brook MP, Dupree DW. Bilateral traumatic chylothorax. Ann Emerg Med. 1988;17:69-72. Â
