- Clinical Technology
- Adult Immunization
- Hepatology
- Pediatric Immunization
- Screening
- Psychiatry
- Allergy
- Women's Health
- Cardiology
- Pediatrics
- Dermatology
- Endocrinology
- Pain Management
- Gastroenterology
- Infectious Disease
- Obesity Medicine
- Rheumatology
- Nephrology
- Neurology
- Pulmonology
A Wide, Slow Cardiac Rhythm in a Lethargic Patient
This 32-year-old woman's family brought her to the ED after 2 days of progressive confusion, fatigue, and weakness. Her multiple medical problems included juvenile-onset diabetes mellitus. Here, more details and a management challenge.
Figure 1.
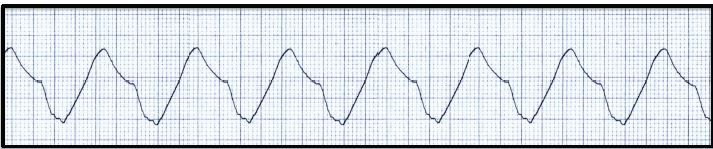
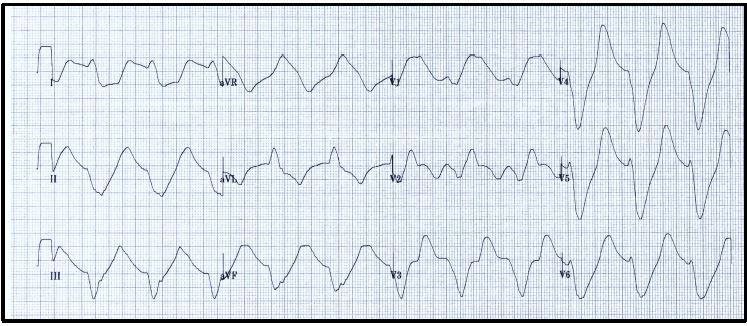
Figure 2.
A 32-year-old woman with multiple medical problems was brought to the emergency department with lethargy and weakness. The family noted progressive confusion and fatigue over 2 days, coupled with extreme weakness. The patient and family denied all other complaints as well as any traumatic or toxicologic events. The medical history included juvenile-onset diabetes mellitus, hypertension, renal insufficiency, and diabetic retinopathy with visual impairment; the patient used insulin and lisinopril as well as several other unknown medications.
On examination, she was confused and lethargic but was aroused by stimuli and spoke coherently. Vital signs were: blood pressure, 188/106 mmHg; pulse, approximately 70 beats/min; respiratory rate, 24 breaths/min; temperature, 36.1°C (97°F); and oxygen saturation, 94% on room air; the ECG monitor demonstrated the rhythm strip in Figure 1. A bedside glucose was 256 mg/dL. The remainder of the examination was unremarkable. Results of a 12-lead ECG are seen in Figure 2.
Based upon the ECG findings noted in Figures 1 and 2, which of the following best describe the patient’s risk of an adverse event and the most appropriate management:
A. Low risk; atropine IV and glucagon IV
B. Intermediate risk; transcutaneous pacing and IV epinephrine infusion
C. High risk; synchronized electrical cardioversion with amiodarone IV
D. Extremely high risk; calcium IV, sodium bicarbonate IV, and dextrose/insulin IV
Please leave below any thoughts you may have on this case.
For answers and discussion, CLICK HERE.
