- Clinical Technology
- Adult Immunization
- Hepatology
- Pediatric Immunization
- Screening
- Psychiatry
- Allergy
- Women's Health
- Cardiology
- Pediatrics
- Dermatology
- Endocrinology
- Pain Management
- Gastroenterology
- Infectious Disease
- Obesity Medicine
- Rheumatology
- Nephrology
- Neurology
- Pulmonology
Use of Digital Twin Technology Enabled Significant HbA1c Reduction and Medication Tapering in Primary Care T2D Management
A Cleveland Clinic trial revealed that AI-driven precision treatment significantly reduced HbA1c and body weight, often eliminating need for medications other than metformin.
A Cleveland Clinic–led randomized clinical trial published in NEJM Catalyst found that an AI-enabled precision treatment system markedly reduced hemoglobin A1c (HbA1c) and reliance on glucose-lowering pharmacotherapy in adults with type 2 diabetes (T2D) treated in primary care.
After 12 months, 71% of participants assigned to the Twin Precision Treatment system achieved an HbA1c below 6.5% while taking only metformin, compared with 2.4% of participants receiving usual care (P <.001).

Lead investigator Kevin M. Pantalone, DO, director of diabetes initiatives at the Cleveland Clinic, and colleagues collaborated with a team of 13 primary care physicians to recruit 150 adults from the Cleveland Clinic Twinsburg Family Health Center, Twinsburg, Ohio. Of these, 100 were randomly assigned to the Twin Precision Treatment group and 50 to the standard of care group. Mean age of the final cohort was 58.5 years and mean duration of T2D was approximately 9 years. The average body mass index (BMI) was 35.1 kg/m2 and average HbA1c level was 7.2%.
The trial’s primary endpoint was the proportion of participants achieving HbA1c of 6.5% or less without use of glucose-lowering medications other than metformin at 12 months. A secondary endpoint included maintaining this target for at least 90 days prior to the 12 month point.
Findings
At one year, Pantalone and colleagues reported, significantly more participants in the intervention group achieved or sustained HbA1c of 6.5% or less for 90 days or more before the 12-month mark and were taking only metformin (52.5% vs 2.8%; P <.001). The mean reduction in HbA1c was −1.3% in the intervention group vs −0.3% in the usual care group (P <.001).
Participants in the intervention group experienced significant declines in use of antihyperglycemic medication, according to the study:
- GLP-1 receptor agonists: 41% to 6%
- SGLT-2 inhibitors: 27% to 1%
- DPP-4 inhibitors: 33% to 3%
- Insulin: 24% to 13%
In total, 85% of participants in the Twin Health group eliminated GLP-1 therapy, according to Twin Health, while mean weight reduction at 12 months was higher in the intervention arm (−8.6%) compared with the usual care arm (−4.6%; P <.001).
“In routine clinical practice, type 2 diabetes is often treated with a one-size-fits-all approach where individuals are prescribed medications and told to ‘watch their diet and stay active,’" Pantalone said in a statement. "Our study demonstrated the AI-enabled system of sensors to understand each patient’s unique metabolic profile, and AI-enabled human care team coaching facilitated significant improvements in glycemic control, weight loss, and quality of life versus usual care, while allowing marked de-escalation of glucose-lowering medications. Interventions like this system can help patients make informed, lasting lifestyle changes to control their blood sugar and sustain weight loss.”
AI-Enabled Data Collection Plus Coaching
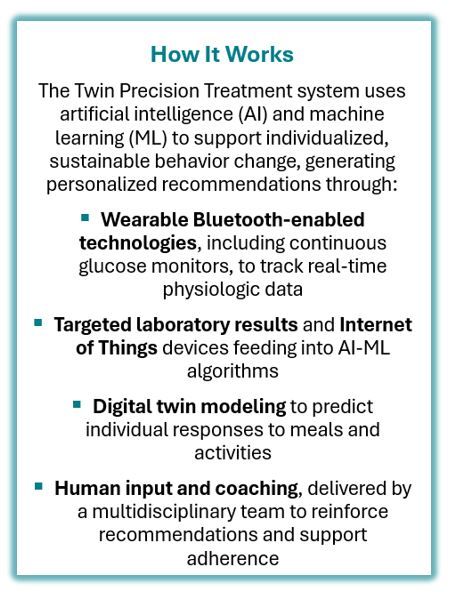
The Twin Precision Treatment combines digital twin AI with personalized clinical care, including licensed providers, nurses, and coaches. Data are collected from wearable sensors that track glucose, weight, blood pressure, activity, sleep, and stress. A smartphone app delivers personalized recommendations on diet and activity, with dietary guidance generated from AI-enabled predictions of glycemic responses to specific meals.
“The study demonstrates that AI-driven precision medicine is the key to metabolic healing,” Lisa Shah, MD, chief medical officer and executive vice president of Twin Health, said in a statement.
Pantalone and the research team found that quality-of-life and treatment satisfaction scores improved significantly from baseline in the intervention group but not in usual care. Exploratory analyses also showed that overall glucose-lowering pharmacotherapy use declined markedly in the intervention group, while it remained stable in usual care.
T2D affects nearly 1 in 10 Americans, and prolonged elevated glucose increases risk for cardiovascular, renal, and neurologic complications. Achieving and maintaining a HbA1c of less than 7, the target recommended by the American Diabetes Association for most adults, can be challenging, however, and the status of HbA1c in the US is described as "suboptimal."
"Optimal glycemic control in T2D remains an elusive goal despite an expanding range of effective treatments and technologies," Pantalone et al wrote in NEJM Catalyst. "Sustained, disciplined adherence to lifestyle modifications leads to positive outcomes in T2D, although converting medical recommendations into effective patient action is challenging in real-world practice.
"The emergence of AI and machine learning (ML) presents innovative opportunities to prompt effective lifestyle modifications and diabetes goal achievements in highly user-specific and user-friendly ways."
The authors note that given the single-center nature of the trial, generalizability may be limited. At the same time they emphasize that the results "highlight the feasibility of incorporating precision digital health approaches into primary care to address persistent challenges in diabetes management."
References
Pantalone KM, Xiao H, Bena J, et al. NEJM Catal Innov Care Deliv. 2025;6(9). doi:10.1056/CAT.25.0016
New peer-reviewed study in New England Journal of Medicine Catalyst finds Twin Health's AI precision treatment significantly improves outcomes in patients with type 2 diabetes and reduces reliance on costly medications, including GLP-1s. News release. Twin Health. August 20, 2025. Accessed August 21, 2025. https://usa.twinhealth.com/resources/cleveland-clinic-study
American Diabetes Association Professional Practice Committee. 6. Glycemic Goals and Hypoglycemia: Standards of Care in Diabetes—2025. Diabetes Care 2025;48(Suppl 1):S128-145. doi:10.2337/dc25-SINT
