- Clinical Technology
- Adult Immunization
- Hepatology
- Pediatric Immunization
- Screening
- Psychiatry
- Allergy
- Women's Health
- Cardiology
- Pediatrics
- Dermatology
- Endocrinology
- Pain Management
- Gastroenterology
- Infectious Disease
- Obesity Medicine
- Rheumatology
- Nephrology
- Neurology
- Pulmonology
GLP-1: Used Only as Needed
The ADA recommends GLP-1 agonists as second-line therapy against type 2 diabetes. What makes this class unique in its impact on hyperglycemia?
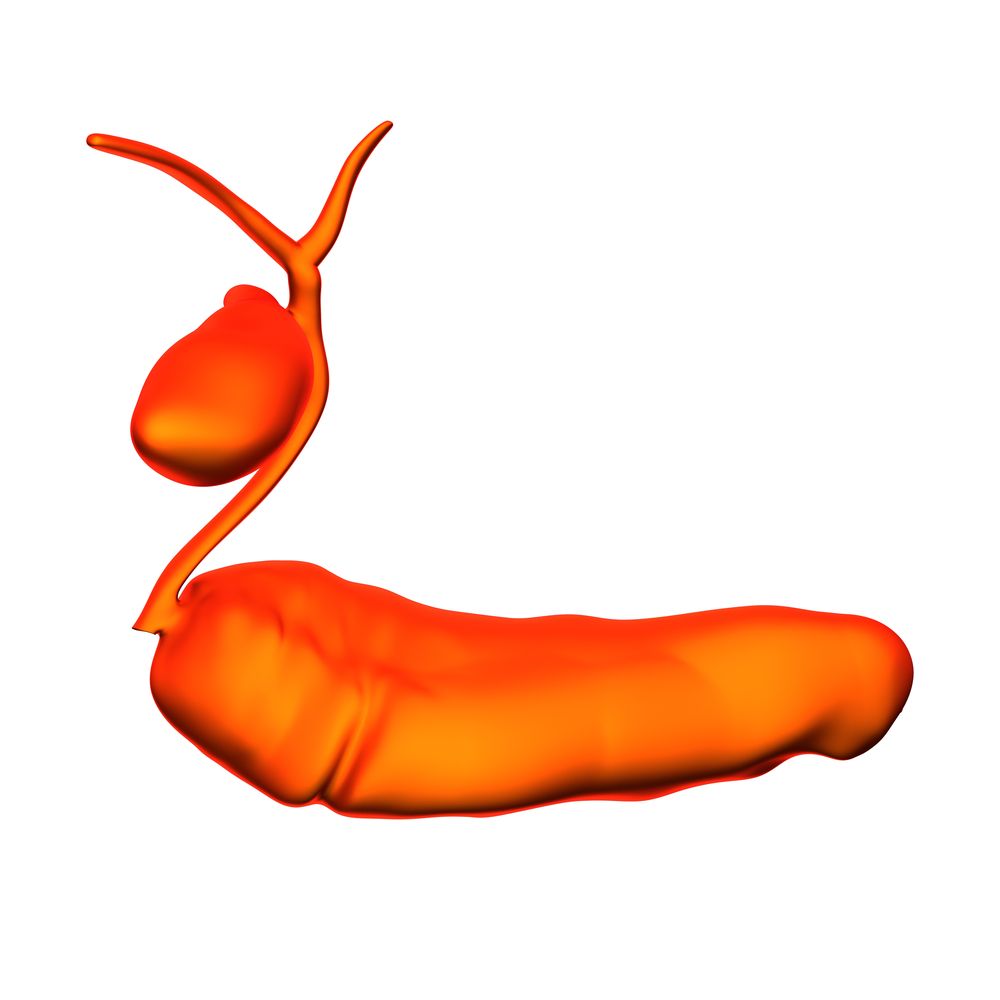
GLP-1 stimulates insulin release only when blood glucose is elevated. ©decade3d-anatomyonline
The American Diabetes Association recommends diet, exercise, and metformin as “first-line” agents in the treatment of type 2 diabetes mellitus (T2DM). As a second line, there are many options-two of them injectable, ie, insulin and glucagon-like peptide-1 (GLP-1) receptor agonists. The GLP-1 agonists are not brand new, but primary care is still testing them out. Test yourself on the class with a short quiz.
1. Which of the following characterize of the hormonal perturbations that occur in T2DM?
A. Less insulin secretion from the pancreas
B. Increased glucagon secretion from the pancreas
C. Attenuated response to insulin in peripheral tissues (ie, liver and muscle cells)
D. A and C
E. All of the above
Please click here for answer, discussion, next question.
Answer: E. All of the above.
The pathogenesis of T2DM and is complex and multifactorial and involves perturbations at many levels of glucose homeostasis, including options 1, 2, and 3 listed above.
2. Which of the following is/are true about the actions GLP-1?
A. GLP-1 stimulates insulin secretion
B. GLP-1 inhibits glucagon secretion
C. GLP-1 secretion from the pancreas is glucose-dependent (ie, in response to a meal)
D. All of the above
E. None of the above
F. It depends on the blood glucose level
Please click here for answer, discussion, next question.
Answer: F. It depends on the blood glucose level.
GLP-1 is secreted by the gut and in response to ingestion of food and has two effects on the pancreas: (1) stimulation of insulin release and (2) inhibition of glucagon secretion from pancreas alpha cells. The glucose-dependent action of endogenous GLP-1 confers a protective effect against hypoglycemia. Therefore, when blood glucose levels are low or normal, GLP-1 secretion is not stimulated; therefore, neither is insulin secretion stimulated or glucagon secretion suppressed. The GLP-1 receptor agonists exploit this homeostatic mechanism to improve glycemic control.
3. What is the most common adverse effect associated with GLP-1 receptor agonists?
A. Headache
B. Dizziness
C. Nausea and gastrointestinal symptoms
D. Transaminitis
Please click here for answer, discussion, next question.
Answer: C. Nausea and gastrointestinal symptoms.
Although adverse effects with this class of drug are relatively rare, there are some individuals who are unable to tolerate the drug at all because of gastrointestinal effects. There are others in whom these effects occur within the first few weeks of treatment but then subside. Although the mechanism is probably multifactorial, it is thought that the nausea and gastrointestinal symptoms associated with GLP-1 agonists are related to the associated delayed gastric emptying and via direct effects on the appetite centers in the hypothalamus.
4. Unlike insulin, GLP-1 agonists do not create the risk for hypoglycemia.
A. True
B. False
Please click here for answer and discussion.
Answer. A. True.
GLP-1 agonists mimic the action of endogenous GLP-1, only stimulating insulin secretion when blood glucose is high and greatly reducing the potential for hypoglycemia. Exogenous insulin, on the other hand, stimulates pancreatic insulin secretion regardless of blood glucose level, posing a significant threat of hypoglycemia. Beware, however, when using GLP-1 agonists in combination with other antidiabetic agents, such as insulin or sulfonylureas. GLP-1 agonists can cause significant hypoglycemia.
Another important difference between these two injectable agents is the impact on body weight with GLP-1 agonists associated with weight loss vs weight gain seen with insulin.
