- Clinical Technology
- Adult Immunization
- Hepatology
- Pediatric Immunization
- Screening
- Psychiatry
- Allergy
- Women's Health
- Cardiology
- Pediatrics
- Dermatology
- Endocrinology
- Pain Management
- Gastroenterology
- Infectious Disease
- Obesity Medicine
- Rheumatology
- Nephrology
- Neurology
- Pulmonology
Gestational Diabetes: Guideline Highlights for Primary Care
New guidelines on gestational diabetes from the American College of Gynecology may be useful for family physicians and others who provide postpartum and primary care for women with GDM.
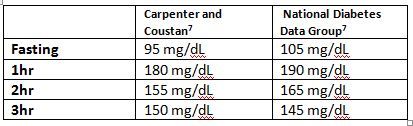
Table. Click to enlarge.
In August 2013, The American College of Obstetricians and Gynecologists (ACOG)1 issued long-awaited practice guideline for gestational diabetes mellitus (GDM), the first update since 2001.
Diabetes develops in roughly 6% to 7% of pregnancies, with approximately 90% of this incidence attributable to GDM, although this varies by patient population, race, and ethnicity. The prevalence of GDM is higher among women of African American, Hispanic, Native American, Asian, and Pacific Islander descent.2
Women with GDM have a 7-fold increased risk for developing T2DM later in life and require lifelong screening for diabetes. About 50% of women with GDM go on to develop T2DM, on average between 22 and 28 years after pregnancy.3,4 Certain ethnic groups are considered at significantly higher risk. For example, up to 60% of Latin American women may develop T2DM 5 years after receiving a diagnosis of GDM.5
A Note for Primary Care
The new ACOG guidelines could be useful to family physicians involved in the initial diagnosis and care of women with GDM, as well as to other clinicians that provide postpartum and long-term health care for women affected by GDM. Recommendations of concern to primary care and other providers are summarized here. Comparisons with recommendations from the American Diabetes Association (ADA)6 also are noted.
DIAGNOSIS
Early Screening
ACOG: Perform in high-risk women with a previous history of GDM, known impaired glucose metabolism, or BMI ≥30; if negative, repeat screening at 24 to 28 weeks’ gestation
ADA: Screen at the ï¬rst prenatal visit in women with risk factors
Standard Screening
ACOG: At 24 to 28 weeks for all pregnant women
ADA: At 24 to 28 weeks for all pregnant women
Screening Tests
ACOG: 2-step approach. First step: 50 g of oral glucose solution and glucose venous blood test at 1 hour. Second step: 100 g 3-hour diagnostic glucose tolerance test
ADA: 1-step approach. 75-g OGTT, with glucose values determined after 8 hours of fasting and at 1 and 2 hours
Diagnostic Cutoffs
ACOG: Because of lack of good-quality comparative trials, clear diagnostic criteria are not available; clinicians should choose 1 of 2 sets (see Table) and consistently follow them, based on their patient population and available resources.
ADA: Fasting 92 mg/dL; 1-hour value 180 mg/dL; 2-hour value 153 mg/dL
MANAGEMENT
The ADA does not give specific recommendations regarding management of GDM. Briefly, ACOG recommends:
Initial management: Nutritional counseling, exercise, blood glucose surveillance
Blood glucose monitoring: Better-quality evidence is needed, but the general recommendation remains 4 times daily taken as fasting, or 1 or 2 hours postprandially.
Insulin: Usual starting threshold fasting > 95 mg/dL; 1-hour levels ≥140 mg/dL; 2-hour levels ≥120 mg/dL; starting dose: 0.7-1.0 units/kg daily in divided doses
Glyburide: Usual starting dose 2.5-20 mg daily in divided doses; likely does cross the placenta, long-term outcomes unknown
Metformin: Most commonly used in women with PCOS or pregestational diabetes, and continued in pregnancy, with the addition of insulin
POSTPARTUM MANAGEMENT AND T2DM PREVENTION
The ADA supports the International Association of Diabetes and Pregnancy Study Groups (IADPSG), recommendation that high-risk women with a diagnosis of diabetes at their first prenatal visit should be considered to have overt T2DM, rather than GDM. ACOG does not address this diagnostic issue, but emphasizes the importance of lifelong screening and prevention of T2DM after GDM has been diagnosed:
Postpartum Screening
ACOG: 6 to 12 weeks postpartum using fasting plasma glucose or 75-g 2-hour OGTT
ADA: 6 to 12 weeks postpartum, using the OGTT and standard adult criteria
Pre-Diabetes/Impaired Glucose Tolerance
ACOG: Annual blood glucose screening; consider referral to specialist, nutritionist, metformin
ADA: Lifestyle modification or metformin
Prevention
ACOG: Blood glucose testing every 3 years; weight loss and physical activity as needed
ADA: Blood glucose screening at least every 3 years
Take-Home Message
While most clinicians may not be involved in the management of pregnancy complicated by GDM, its effects are lifelong. In that sense, discussing a history of GDM, as well as the increased risk for T2DM, is within the purview of all health care providers.
References:
- The American College of Obstetricians and Gynecologists. Practice Bulletin No. 137: Gestational Diabetes Mellitus. Obstetrics & Gynecology. Obstet Gynecol. 2013;122:406-416. doi: 10.1097/01.AOG.0000433006.09219.f1
- Wier LM, Witt E, Burgess J, Elixhauser A. Hospitalizations Related to Diabetes in Pregnancy, 2008. HCUP Statistical Brief #102. Rockville, MD: Agency for Healthcare Research and Quality; 2010. http://www.hcup-us.ahrq.gov/reports/statbriefs/sb102.pdf. Accessed February 14, 2014.
- England LJ, Dietz PM, Njoroge T, et al. Preventing type 2 diabetes: public health implications for women with a history of gestational diabetes mellitus. Am J Obstet Gynecol. 2009;200:365.e1–e8.
- O’Sullivan JB. Body weight and subsequent diabetes mellitus. JAMA. 1982;248:949–952. (Level II-2)
- Kjos SL, Peters RK, Xiang A, et al. Predicting future diabetes in Latino women with gestational diabetes. Utility of early postpartum glucose. Diabetes. 1995;44:586-591.
- American Diabetes Association. Standards of Medical Care in Diabetes. Diabetes Care. 2013;36(suppl 1):S-e4.
- Berggren EK, Boggess KA, Stuebe AM, Jonsson Funk M. National Diabetes Data Group versus Carpenter-Coustan Criteria to diagnose gestational diabetes. Am J Obstet Gynecol. 2011;205:253.e1–253.e7. doi:10.1016/j.ajog.2011.06.026. Full text available at: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3670957/pdf/nihms-474230.pdf
