
- Clinical Technology
- Adult Immunization
- Hepatology
- Pediatric Immunization
- Screening
- Psychiatry
- Allergy
- Women's Health
- Cardiology
- Pediatrics
- Dermatology
- Endocrinology
- Pain Management
- Gastroenterology
- Infectious Disease
- Obesity Medicine
- Rheumatology
- Nephrology
- Neurology
- Pulmonology
Fatal Progressive Multifocal Leukoencephalopathy: Still a Problem in the Era of Highly Active Antiretroviral Therapy
A 37-year-old white woman, previously in excellent health, presented to a local emergency department for evaluation of evolving left-sided weakness and a slight left facial droop.
A 37-year-old white woman, previously in excellent health, presented to a local emergency department for evaluation of evolving left-sided weakness and a slight left facial droop. Findings from her general medical examination were unremarkable, but a neurological examination documented a left homonymous hemianopia, left hemiparesis, and hyperreflexia. Laboratory studies revealed mild pancytopenia, normal hepatic transaminase levels, normal serum lactate dehydrogenase level, and iron indices consistent with anemia of chronic disease.
The patient's MRI scans showed abnormal signal in subcortical white matter of the right cerebral occipital/temporal regions on fluid-attenuated inversion recovery (FLAIR)/T2-weighted images (ie, weighting schematic for MRI in which damaged tissues are hyperintense). Although malignancy was considered, the MRI findings were most consistent with progressive multifocal leukoencephalopathy.
Information obtained in the patient's history was unremarkable, without any injection drug use or other notable risk factors for HIV infection. She had a total of 3 heterosexual partners; her current partner had recently tested negative, and her former husband reported a negative HIV test result on insurance screening 3 years ago.
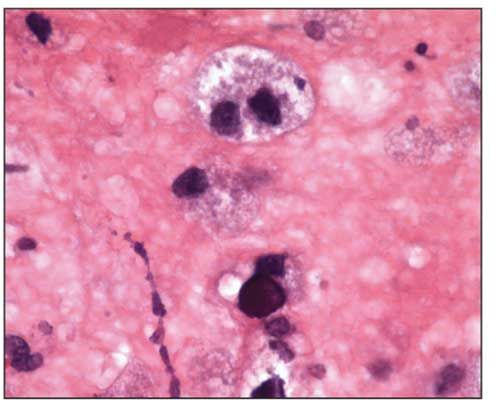
Figure 1. Brain biopsy sample showing central oligodendrocyte with viral inclusion bodies giving a smudged appearance to nucleus. At other foci, enlarged, bizarre eosinophilic astrocytes were abundant. Confirmation of JC virus infection involved additional immunohistochemical analysis (hematoxylin and eosin stain, original magnification ×1000).
Evaluation of a bone marrow aspirate revealed a paucity of lymphocytes, and a CD4+ cell count of less than 50/μL prompted an HIV enzyme-linked immunosorbent assay, followed by a confirmatory Western blot test. Her HIV-1 RNA level was 88,000 copies/mL. Results of testing for hepatitis virus, cytomegalovirus, and herpes virus were negative. Cerebrospinal fluid (CSF) polymerase chain reaction (PCR) was positive for JC virus (JCV) RNA. Brain biopsy confirmed the diagnosis of progressive multifocal leukoencephalopathy (PML) (Figure 1).
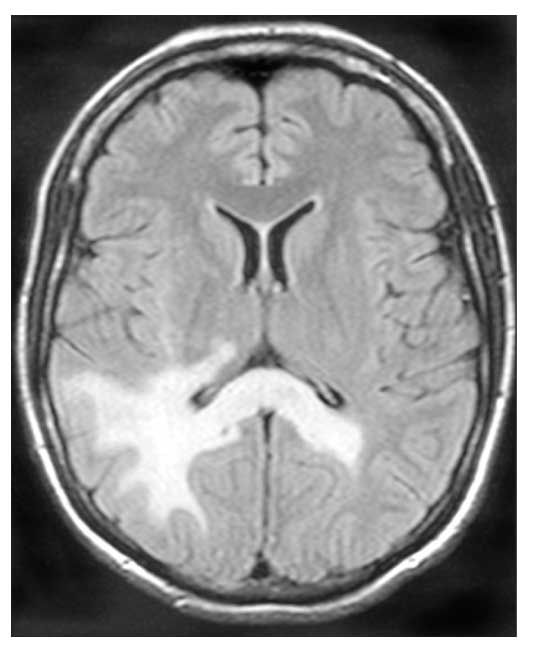
Figure 2. Brain MRI scan at presentation displays signal abnormalities on fluid-attenuated inversion recovery/T2-weighted sequence. Lesions involve the temporal/occipital lobes and corpus callosum. Lesions are hyperintense on the T2-weighted image. There was no abnormal enhancement with gadolinium, and no mass effect.
An antiretroviral regimen of tenofovir, emtricitabine, and lopinavir/ritonavir was started. Within 4 weeks, the patient's HIV-1 RNA level declined to less than 75 copies/mL. However, her CD4 count did not improve over a 2-month period. Clinical deterioration was heralded by worsening left-sided weakness and the sudden development of blindness. Serial brain MRI scans obtained over a 45-day period showed extensive progression of the lesions that accompanied the neurological changes (Figures 2 and 3). Immune reconstitution inflammatory syndrome (IRIS) was considered, although many diagnostic features were not present; however, neurological deterioration prohibited additional brain biopsies. Nevertheless, glucocorticoid treatment was initiated but without success. The patient experienced progressive weakness and died of respiratory failure 3 months after her initial MRI.
Early initiation of antiretroviral therapy remains the foundation of treatment for HIV-associated PML. Despite improvements in antiviral treatments, the prevalence of PML remains unchanged at 5% in HIV-positive patients.1 Furthermore, while morbidity and mortality have improved, estimated mortality is 50% at 1 year in those who are receiving antiretroviral therapy,2 and 80% of patients will retain some degree of neurological deficit.3
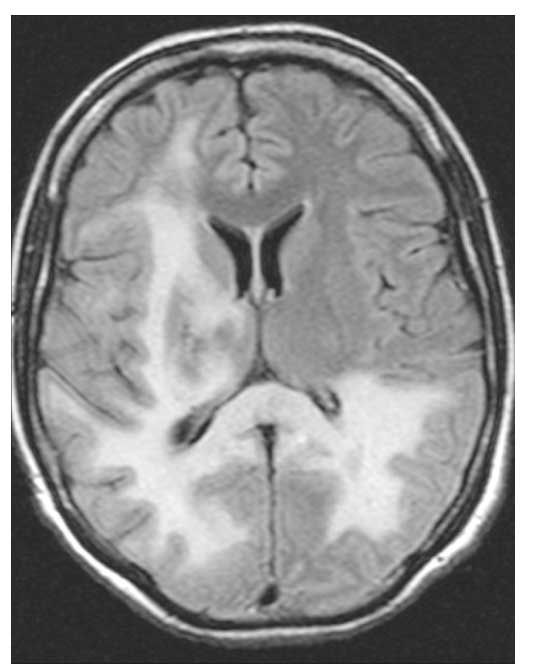
Figure 3. Brain MRI scan obtained 2 months after initial MRI demonstrates involvement of frontal lobe, thalamus, and near-complete bilateral occipital involvement. Not shown here is the vertical spread of pons, midbrain, and cerebellum that was present.
Diagnosis of PML is based on clinical findings, neuroradiographic imaging, and virological testing. Fifty-three percent of patients with PML present with hemiparesis, and 43% present with cognitive impairment. Other, less frequent presentations include speech or visual deficits, ataxia, and seizures.4 Classic MRI findings are well-demarcated, asymmetric lesions in periventricular and subcortical white matter. The lesions are characteristically hyperintense on FLAIR/T2-weighted images, hypointense on T1-weighted images, and non-enhancing with gadolinium and do not create mass effect.4 JCV DNA can often be isolated from CSF by PCR. However, early use of antiretroviral therapy may allow rapid CSF clearance, and the sensitivity of CSF PCR in some studies is estimated to be as low as 53%.3 Brain biopsy is the gold standard for diagnosis of PML, with tissue samples showing JCV infection of oligodendrocytes, associated demyelination, and reactive changes.3
IRIS will develop in 10% of patients with PML, and their presentation will deviate from the classic presentation.4 Immune reconstitution, particularly when initial CD4+ cell counts are less than 50/μ L and the HIV RNA level rapidly declines, can contribute to clinical worsening of PML.5 On MRI, IRIS is associated with significant gadolinium enhancement, presumably representing the breakdown of the blood-brain barrier because of the action of inflammatory cells.6 Findings from a confirmatory brain biopsy reveal perivascular lymphocytic infiltration of primarily CD8+ cells, in addition to JCV.3 Typically, PML-associated IRIS follows a milder course, and the presence of gadolinium enhancement has been associated with improved prognosis.2
Besides the development of IRIS, determinants of the clinical course of PML are still being delineated. Du Pasquier and colleagues2 describe a differential progression of disease and survival related to the presence of JCV-specific CD8+ cells (cytotoxic lymphocytes); they estimated a positive predictive value of 82% for evolution of aggressive PML in patients without JCV-specific cytotoxic lymphocytes.
Our case serves to remind clinicians that PML remains a significant infection among HIV-infected persons and a source of great morbidity and occasional mortality even with the availability of effective antiretroviral therapy.
Acknowledgment: The authors wish to thank Dr Nick Agoff for cytopathological review of the images and Dr David Coy for radiographic interpretation.
References:
References
1.
Wyen C, Hoffmann C, Schmeisser N, et al. Progressive multifocal leukoencephalopathy in patients on highly active antiretroviral therapy: survival and risk factors of death.
J Acquir Immune Defic Syndr
. 2004;37:1263-1268.
2.
Du Pasquier RA, Kuroda MJ, Zheng Y, et al. A Prospective study demonstrates an association between JC virus-specific cytotoxic T lymphocytes and the early control of progressive multifocal leukoencephalopathy.
Brain
. 2004;127(pt 9):1970-1978.
3.
Koralnik IJ. Progressive multifocal leukoencephalopathy revisited: has the disease outgrown its name?
Ann Neurol.
2006;60:162-173.
4.
Weber T. Progressive multifocal leukoencephalopathy.
Neurol Clin
. 2008;26:833-854, x-xi.
5.
Riedel DJ, Pardo CA, McArthur J, Nath A. Therapy insight: CNS manifestations of HIV-associated immune reconstitution inflammatory syndrome.
Nat Clin Pract Neurol
. 2006;2:557-565.
6.
Safdar A, Rubocki RJ, Horvath JA, et al. Fatal immune restoration disease in human immunodeficiency virus type 1-infected patients with progressive multifocal leukoencephalopathy: impact of antiretroviral therapy-associated immune reconstitution.
Clin Infect Dis
. 2002;35:1250-1257.
FDA Approves First Oral GLP-1 Receptor Agonist for Chronic Weight Management
December 23rd 2025The FDA approved once-daily oral semaglutide 25 mg for chronic weight management and long-term weight maintenance in adults with obesity or overweight, based on data from the OASIS clinical trial program.
Phase 3 Data Support Oral Orforglipron for Weight Maintenance After GLP-1–Based Weight Loss
December 19th 2025Topline Phase 3 ATTAIN-MAINTAIN data show oral orforglipron met primary and key secondary endpoints for weight maintenance after prior GLP-1–based injectable therapy in adults with obesity.
FDA Approves First Oral GLP-1 Receptor Agonist for Chronic Weight Management
December 23rd 2025The FDA approved once-daily oral semaglutide 25 mg for chronic weight management and long-term weight maintenance in adults with obesity or overweight, based on data from the OASIS clinical trial program.
Phase 3 Data Support Oral Orforglipron for Weight Maintenance After GLP-1–Based Weight Loss
December 19th 2025Topline Phase 3 ATTAIN-MAINTAIN data show oral orforglipron met primary and key secondary endpoints for weight maintenance after prior GLP-1–based injectable therapy in adults with obesity.
2 Commerce Drive
Cranbury, NJ 08512
All rights reserved.