- Clinical Technology
- Adult Immunization
- Hepatology
- Pediatric Immunization
- Screening
- Psychiatry
- Allergy
- Women's Health
- Cardiology
- Pediatrics
- Dermatology
- Endocrinology
- Pain Management
- Gastroenterology
- Infectious Disease
- Obesity Medicine
- Rheumatology
- Nephrology
- Neurology
- Pulmonology
Asthma May be Linked to Severe COVID-19 but Not to Risk for Hospitalization
Patients with asthma who did require hospitalization for SARS-CoV-2 infection were at greater risk for intubation and remdesivir treatment, a new study reports.
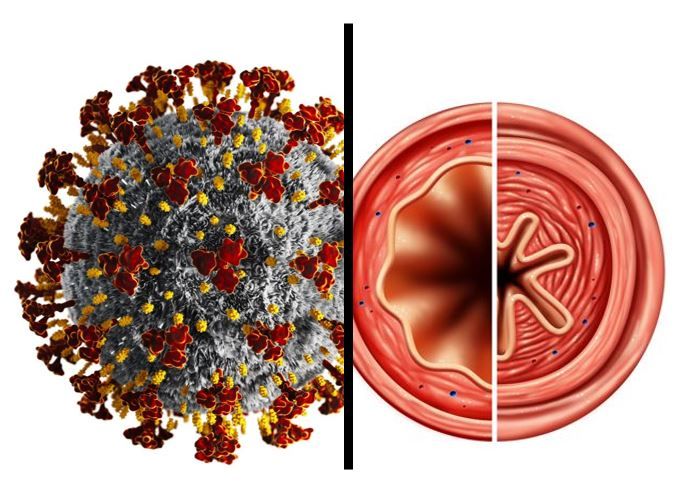
Asthma was not associated with increased risk of hospitalization for COVID-19 but patients with asthma who were hospitalized were at risk for more severe disease, in findings from a new study by researchers from Kaiser Permanente (KP) Northern California.
Specifically, asthma patients hospitalized for COVID-19 were at increased risk for ICU admission, intubation, and treatment with remdesivir.
The study results are being presented at the American Association of Allergy, Asthma & Immunology (AAAAI) 2022 Annual Meeting, held in Phoenix, Arizona, from February 25 to 28.
Citing the limited knowledge about asthma as a risk factor for COIVD-19, the KP investigators conducted a retrospective cohort study that compared the incidence of COVID-19 infection, hospitalization, and severity of COVID-19 during 2020 in a large group (n = 41,282) of adult patients with asthma and a control group of the same size matched for age, sex, and race/ethnicity. Mean age of the combined cohorts was 55 years; 63% were female, and 55% were White. The researchers used electronic health records to collect data on demographics, clinical factors, comorbidities, polymerase chain reaction COVID-19 testing, hospitalization, and inpatient COVID-19 treatment.
After multivariable adjustment investigators found that asthma was inversely associated with having a positive COVID-19 test (8.7 vs 9.4% positive among those tested; OR=0.90; 95% CI, 0.82-0.99; p=0.03). Specific adjustments were for age, sex, race/ethnicity, BMI, smoking, Neighborhood Deprivation Index, and comorbidities.
After adjusting for the same covariates in each instance, Asthma was not associated with COVID-19 hospitalization (2.9 vs 1.4 per 1,000 persons; OR=1.04; 95% CI, 0.96-1.12; p 0.32) but having asthma was positively associated with a composite outcome of COVID-19-related ICU admission, intubation, or remdesivir treatment (2.5 vs 1.0 per 1,000 persons; OR=1.89; 95% CI, 1.28-2.81; p=0.001).
Based on these results the authors conclude that “asthma may be a risk factor for severe COVID-19” even though in this analysis it was associated with lower odds of virus infection and not independently associated with risk for hospitalization.
Reference: Finkas LK, Block L, Lu M, et al. Retrospective analysis of COVID-19 incidence and health outcomes among patients with asthma in a large integrated health care delivery system. Presented at: American Academy of Allergy, Asthma & Immunology (AAAAI) 2022 Annual Meeting; February 25–28, 2022; Phoenix, AZ. Abstract 171.
Kymera's Oral STAT6 Degrader KT-621 Shows Biologic-Like Activity in Early Atopic Dermatitis Trial
December 8th 2025KT-621 achieved deep STAT6 degradation and strong 4-week EASI and itch reductions, offering a potential new oral option for moderate–severe AD and other Th2 inflammation-driven disease.
