- Clinical Technology
- Adult Immunization
- Hepatology
- Pediatric Immunization
- Screening
- Psychiatry
- Allergy
- Women's Health
- Cardiology
- Pediatrics
- Dermatology
- Endocrinology
- Pain Management
- Gastroenterology
- Infectious Disease
- Obesity Medicine
- Rheumatology
- Nephrology
- Neurology
- Pulmonology
5 Seasonal Ills Spawned by Summer
Asthma and allergy symptoms, lupus, Lyme disease, Rocky Mountain spotted fever, southern tick–associated rash illness-several seasonal disorders are brought to light in this concise slideshow.
Asthma and allergy symptoms, cutaneous lupus, Lyme disease, Rocky Mountain spotted fever, southern tick–associated rash illness-several seasonal disorders are brought to light in this concise slideshow.
1. Asthma and Allergy Symptoms Heat Up With Summer Sun
• Asthma and allergy symptoms may be triggered by constant changes in air quality and an abundance of pollen, especially in the summer heat. Control allergen-induced asthma by reducing exposure to the offending substances.
• Determine the patient’s exposure to allergens and sensitivity to the allergens. Use the medical history to determine sensitivity to seasonal allergens, use skin testing or in vitro testing to determine the presence of specific IgE antibodies to perennial indoor allergens, and assess the clinical significance of positive allergy tests in the context of the patient’s medical history.
• Asthma symptoms may be precipitated by exposure to increased air pollution levels. Patients should avoid exertion or outdoor exercise as much as possible when levels of air pollution are high.
NEXT CASE »
For the discussion, click here.

2. Lupus Now Appearing in Sun-exposed Areas Near You
• This mildly pruritic and nontender rash erupted on a 58-year-old woman in late August. She had not started any new ot taking photosensitizing drugs.
• Subacute cutaneous lupus erythematosus (SCLE) was the diagnosis. SCLE presents as nonindurated, nonscarring, erythematous plaques, possibly with a fine scale that may progress into a diffuse, widespread, papulosquamous or annular lesion with central hypopigmentation or telangiectasia.
• SCLE characteristically appears on sun-exposed areas (eg, the vee area of the neck, upper trunk) but spares the knuckles and the face.
• The disease is predictably worse during the spring and summer and may be exacerbated by photosensitizing drugs. The mainstay of treatment is sun protection and avoidance.
NEXT CASE »
For the discussion, click here.

3. Lyme Hits the “Bull’s-eye” in Early Summer
• An otherwise healthy 4-year-old boy who plays outdoors daily had a rash on his left shoulder. He had felt a “scab” there and picked off what probably was a tick. The diagnosis: Lyme disease.
• Lyme disease typically occurs in late spring and early summer. The rash represented early localized infection with the spirochete Borrelia burgdorferi, which manifests as erythema chronicum migrans, an expanding, erythematous, annular rash that sometimes exhibits complete or partial central clearing.
• The classic “bull’s-eye” rash of early localized Lyme disease may be associated with constitutional symptoms (eg, fever, chills, myalgias, and malaise).
• Diagnosis is made clinically on the basis of symptoms and travel to or residence in an area in which Lyme disease is endemic. Serological testing may be needed for diagnosis in the later stages.
NEXT CASE »
For the discussion, click here.

4. Summer Fever: Outdoor Activity Spawns Tick-borne Disease
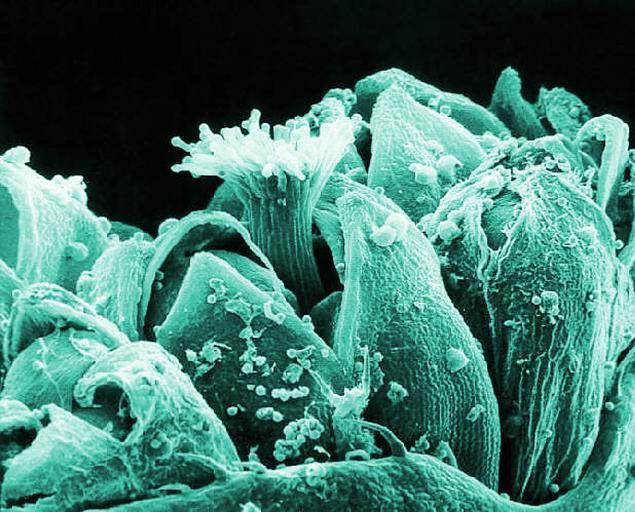
• This patient has Rocky Mountain spotted fever (RMSF). Most infections occur during the spring and summer, when frequent outdoor activity coincides with more adult and nymphal ticks.
• The responsible pathogen is Rickettsia rickettsii, a gram-negative, obligate intracellular bacterium. RMSF is the most common rickettsial infection in the United States.
• Up to one-third of patients with confirmed RMSF do not recall a recent tick bite or tick contact. Symptoms appear 2 to 14 days after exposure. A rash usually develops between the third and fifth days.
• The diagnosis is largely clinical, especially in the early stages, when there is no reliable diagnostic test. Later, the diagnosis can be made by skin biopsy or serology. Timely treatment is crucial.
NEXT CASE »
For the discussion, click here.


5. Tick Bite Brings STARI Nights, and Days
• Early localized Lyme disease was the diagnosis, but further review revealed that the removed tick had a white spot on its dorsum characteristic of Amblyomma americanum (Lone Star tick)(B).
• The Lone Star tick has been implicated as a cause of southern tick–associated rash illness (STARI). STARI presents similarly to Lyme disease, with a target-like rash around the site of a tick bite.
• Patients with STARI may present with fever, headache, fatigue, and muscle and joint pain, although they tend to be less symptomatic and recover more quickly than patients with Lyme disease.
• Differentiation of STARI from Lyme disease on the basis of early clinical signs alone is unreliable, but STARI is not associated with later complications-eg, arthritis, carditis-seen in Lyme disease.
