- Clinical Technology
- Adult Immunization
- Hepatology
- Pediatric Immunization
- Screening
- Psychiatry
- Allergy
- Women's Health
- Cardiology
- Pediatrics
- Dermatology
- Endocrinology
- Pain Management
- Gastroenterology
- Infectious Disease
- Obesity Medicine
- Rheumatology
- Nephrology
- Neurology
- Pulmonology
Young Woman With "Funny" Mole
A 24-year-old woman presented with a chief complaint: “Check a funny mole.” Her boyfriend pointed out that a single mole on her back looked “different.”
A 24-year-old woman presented with a chief complaint: “Check a funny mole.” Her boyfriend pointed out that a single mole on her back looked “different.” The patient denied bleeding, itching, or any other symptoms associated with the lesion in question. Because of its location on the mid-back, she was unable to offer any assessment regarding recent growth or alterations in gross appearance. Her family history was negative for melanoma, although both parents had been treated for non-melanoma skin cancer.
The patient was born and raised in Texas, but denied a history of frequent sunburn. She did not patronize a tanning salon. The patient was in good health.
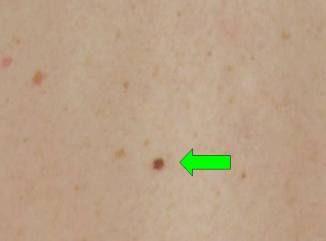
The mole of concern is shown, both from distance and close-up views. Even casual visual inspection disclosed the lesion to be clearly much darker than her other nevi.

How would you approach this problem?
A. Immediately remove this obvious melanoma with 2-cm surgical margins.
B. Immediately remove this obvious melanoma with 2-cm margins and concurrently obtain a serum LDH level, a chest radiograph, and PET scan to evaluate the gravity of the situation.
C. Examine the mole with a dermatoscope and allow it to remain in place if the dermatoscopic findings were not unequivocal for malignancy.
D. Examine the mole with a dermatosocope to rule out melanoma. If the dermatoscopic findings were not conclusive for melanoma, remove the lesion with narrow surgical margins, sending the specimen for histologic evaluation.
E. Treat the lesion with liquid nitrogen cryosurgery.
Click here for the correct answer.
Correct answer: D
This scenario is not uncommon, played out in both dermatology and primary care offices all across the country. Despite technological advances (such as computer-assisted image analysis1), the “well-trained eye” is still best able to discern which pigmented lesions are at high risk. Use of the ABCDE paradigm, while not totally accurate, is quite helpful in sorting through the myriad of pigmented lesions seen by health care professionals.2,3
The lesion of concern in this case demonstrates slight irregularity of border with small “notches” and a hint of color variation, but not much else. It is clearly not an “obvious melanoma,” and an aggressive approach is simply not justifiable.
On the other hand, the lesion is overtly different from the remainder of the patient’s additional nevi-a fact recognized by both lay people (boyfriend, patient) and professionals (dermatology consultant). A previous study verified that identification of outlier lesions based on gross morphology is not difficult.4 The most important point is this: most melanomas do present as outliers, as lesions with a distinctly different appearance than other pigmented lesions on any given individual. Thus, the “ugly ducking” lesion should always at least be considered for biopsy or, alternatively, for conservative removal.5
Dermoscopy consists of the evaluation of pigmented (and other) skin lesions by viewing them magnified and illuminated by polarized light. Based on specific patterns and features recognized during dermatoscopic examination, melanocytic lesions can be classified as unequivocally benign, suspicious, or overtly malignant. Benign lesions can be monitored, suspicious lesions should be biopsied or removed, and malignant-appearing lesions should be removed appropriately. Dermatoscopic examination of pigmented lesions increases diagnostic accuracy by up to 30% compared with examination by the naked eye under normal ambient light.6 A single training course coupled with routine use of the dermatoscope greatly decreases the likelihood that primary care health care professionals will miss the diagnosis of melanoma.7
For this patient, the uniqueness of the lesion dictates that, at a minimum, a biopsy should be performed. With such a small lesion in a relatively non-sensitive cosmetic area, conservative complete removal might be considered a sensible and preferable approach. A dermatoscopic examination would most likely distinguish between merely a suspicious lesion (suitable for biopsy or conservative removal) and a malignancy (subject to removal with wide margin). Thus, a dermatoscopic examination should precede surgical intervention.
References:
1. Jamora MJ, Wainwright BD, Meehan SA, et al. Improved identification of potentially dangerous pigmented skin lesions by computerized image analysis. Arch Dermatol. 2003;139:195-198.
2. Rigel DS, Russak J, Friedman R. The evolution of melanoma diagnosis: 25 years beyond the ABCDs. CA Cancer J Clin. 2010;60:301-316.
3. Aldridge RB, Zanotto M, Ballerini L, et al. Novice identification of melanoma: not quite as straightforward as the ABCDs. Acta Derm Venereol. 2011;91:125-130.
4. Scope A, Dusza SW, Halpern AC, et al. The “ugly duckling” sign: agreement between observers. Arch Dermatol. 2008;144:58-64.
5. Goodson AG, Grossman D. Strategies for early melanoma detection: approaches to the patient with nevi. J Am Acad Dermatol. 2009;60:719-735.
6. Pluddemann A, Heneghan C, Thompson M, et al. Dermoscopy for the diagnosis of melanoma. Br J Gen Pract. 2011;61:416-417.
7. Argenziano G, Puig S, Zalaudek I, et al. Dermoscopy improves accuracy of primary care physicians to triage lesions suggestive of skin cancer. J Clin Oncol. 2006;24:1877–1882.
Atopic Dermatitis: The Pipeline and Clinical Approaches That Could Transform the Standard of Care
September 24th 2025Patient Care tapped the rich trove of research and expert perspectives from the Revolutionizing Atopic Dermatitis 2025 conference to create a snapshot of the AD care of the future.
