- Clinical Technology
- Adult Immunization
- Hepatology
- Pediatric Immunization
- Screening
- Psychiatry
- Allergy
- Women's Health
- Cardiology
- Pediatrics
- Dermatology
- Endocrinology
- Pain Management
- Gastroenterology
- Infectious Disease
- Obesity Medicine
- Rheumatology
- Nephrology
- Neurology
- Pulmonology
When Confronted with Atypical Headache, You May Have to SNOOP
Throbbing occipital headache x2 wks; abrupt onset, no history. Reason for alarm? Neurologist Peter McAllister, MD, suggests you SNOOP first.
Dr McAllister is Medical Director at the New England Institute for Neurology and Headache and Chief Medical Officer for the New England Institute for Clinical Research and Ki Clinical Research, all in Stamford, Conn.
The great majority of headaches primary care providers will see in their office will be primary in nature – migraine, tension type, and cluster being the big 3. However, secondary headaches (in which the pain is generated by something ominous and potentially life-threatening) are lurking out there, and missing one could be disastrous. Consider the following case:
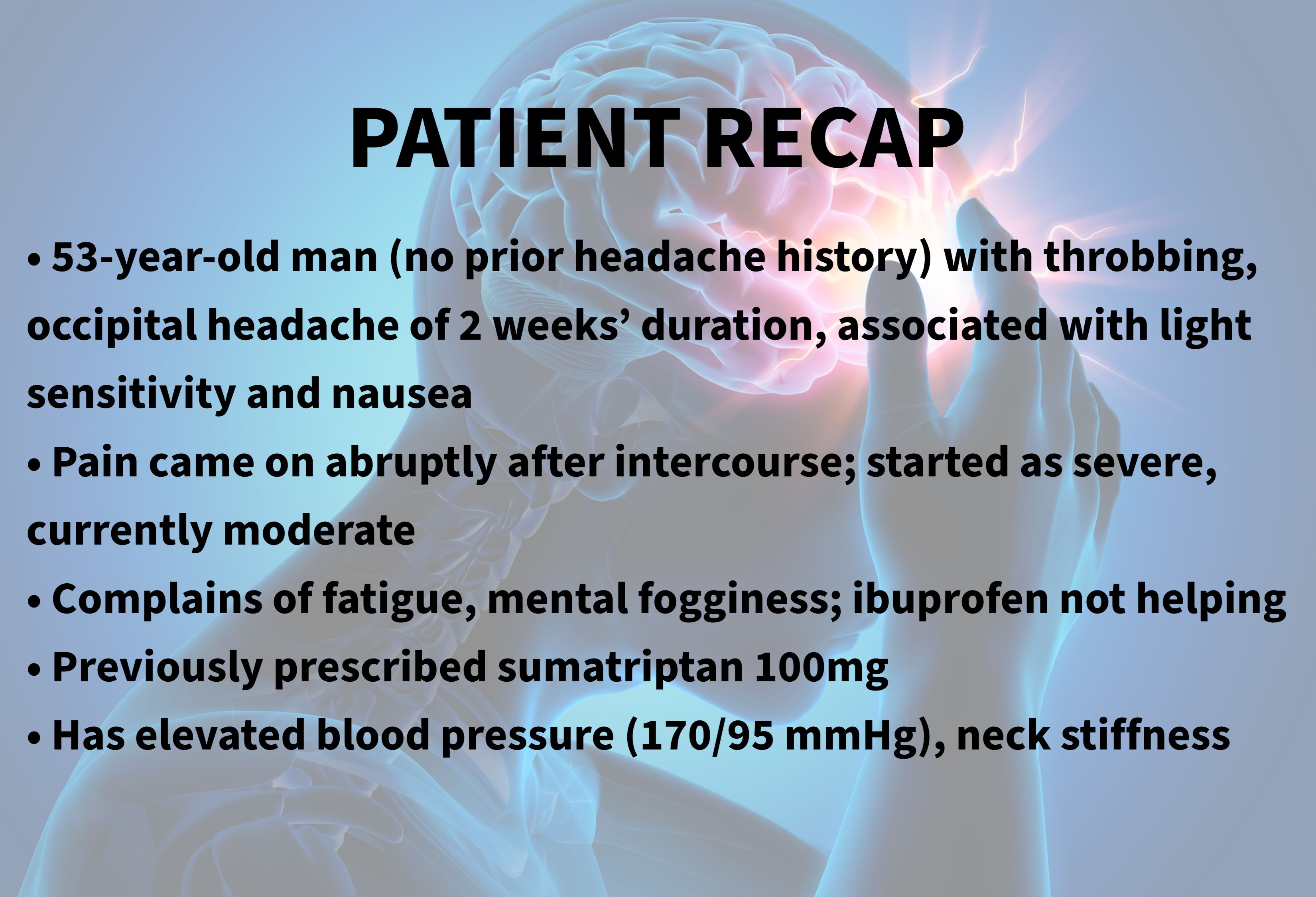
A 53-year-old man presents with a throbbing, occipital headache of 2 weeks’ duration, associated with light sensitivity and nausea. He has no prior headache history. The pain came on abruptly after intercourse, starting out as severe and currently of moderate severity. He also complains of fatigue and mental fogginess. Ibuprofen has not helped. A physician at a walk-in center suggested this was migraine, and prescribed sumatriptan 100mg, which has helped some. Exam is remarkable for elevated blood pressure (170/95 mmHg) and neck stiffness.
Should you:
A. Concur that it is likely migraine and continue the sumatriptan
B. Refer to neurology (who are several months booked out)
C. Apply the SNOOP mnemonic and take appropriate action
If you chose C, congratulations, for SNOOP has proven itself very useful since the American Headache Society brought it out a dozen years ago. SNOOP is the most useful mnemonic in headache medicine, and one well worth committing to memory. SNOOP helps the busy clinician remember the hallmarks of secondary headaches – it facilitates medical decision making, and informs us of when to relax and when to sweat in the face of an unusual headache.
©peterschreiber.media/stock.adobe.com

S is for systemic. This refers to symptoms such as fever, chills, rapid weight loss, and weakness that do not ordinarily occur in primary headaches. It also refers to pre-existing systemic illness with a new headache. For example, a new headache in a cancer or HIV patient (2 systemic illnesses) should be considered secondary until proven otherwise.
N is for neurologic – signs and symptoms, that is. Any focal deficit or patient-reported complaint (eg, weakness, sensory or visual loss, ataxia, and encephalopathy) should cause concern and generate a work-up. Vascular, neoplastic, infectious, and autoimmune culprits can present with headache and focal neurologic deficits.
O is for onset – how quickly the headache sets in. Fast-onset (or quick time from mild to severe pain, say over seconds to minutes) can point to a vascular headache such as a subarachnoid bleed, stroke, or even reversible cerebral vasoconstriction syndrome. Migraine, on the other hand, usually builds to maximal intensity over hours.
O(#2) is for older age. Any new headache after age 50 should prompt at least a thought about a work-up such as imaging or laboratory studies. Giant cell arteritis, subdural hematomas, and tumors commonly strike older patients.
And finally, P is for prior headache history. If a patient has a long history of a primary headache, as long as the current headache is similar, you can breathe easy. Conversely, a patient without a headache history, or a new headache in someone with a headache history, should get your detective skills going. To get fancy, we can add more Ps: Papilledema, pulsatile tinnitus, positional provocation, precipitated by exercise – all of which may be additional clues to unearthing a secondary headache.
©peterschreiber.media/stock.adobe.com
Now back to our case
Thoughtfully reviewing that history and those physical findings, some SNOOPING around (or SNOOPPPPPing, if you add those extra Ps) is clearly warranted.
Your patient comes up positive for 2 Os (abrupt onset, and age >50 years), as well as S for systemic (fatigue, elevated blood pressure, mental fogginess) and N (neck stiffness). He even qualifies for the last P (precipitated by exercise – or in this case intercourse).
You send him for emergent head CT scan, which reveals a posterior subarachnoid hemorrhage with intraventricular extension. Brain MRI and circle of Willis MRA show a likely ruptured posterior communicating artery aneurysm with early vasospasm. The patient is admitted to the intensive care unit, and with proper care, does very well.
There is another useful pearl buried in this case: Aneurysmal rupture headaches often feel better with triptans, as was the case here. Stating it differently: Response to a triptan does not rule in a migraine or rule out a secondary headache.
Your patient survived a potentially catastrophic event because of you, your clinical skills, and a little SNOOPing around.
Suggested Reading:
- Loder E, Weizenbaum E, Frishberg B, Silberstein S, American Headache Society Choosing Wisely Task Force. Choosing wisely in headache medicine: the American Headache Society’s list of five things physicians and patients should question. Headache. 2013;53:1651-1659.
- American College of Emergency Physicians. Clinical policy: critical issues in the evaluation and management of patients presenting to the emergency department with acute headache. Ann Emerg Med. 2002;39:108-122.
- MacGrory B, Vu L, Cutting S, et al. Distinguishing characteristics of headache in nontraumatic subarachnoid hemorrhage. Headache. 2018;3:364-370.
- Dodick D. Headache as a symptom of ominous disease. What are the warning signals? Postgrad Med. 1997;101:46-50,55-56,62-64.
- Locker TE, Thompson C, Rylance J, Mason SM. The utility of clinical features in patients presenting with nontraumatic headache: an investigation of adult patients attending an emergency department. Headache. 2006;46:954-961.Dr McAllister is Medical Director at the New England Institute for Neurology and Headache and Chief Medical Officer for the New England Institute for Clinical Research and Ki Clinical Research, all in Stamford, Conn.
