- Clinical Technology
- Adult Immunization
- Hepatology
- Pediatric Immunization
- Screening
- Psychiatry
- Allergy
- Women's Health
- Cardiology
- Pediatrics
- Dermatology
- Endocrinology
- Pain Management
- Gastroenterology
- Infectious Disease
- Obesity Medicine
- Rheumatology
- Nephrology
- Neurology
- Pulmonology
Temporal Arteritis in a 69-Year-Old Man With Severe Headaches and Right Inferior Homonymous Quadrantopsia
A review of visual field defects including optic atrophy from temporal arteritis, homonymous hemianopic quadrantopsia, and normotensive glaucoma.
The visual pathway extends like a roadway from the retina to the occipital pole. Any interruption of this roadway results in a visual field defect.
VISUAL FIELD DEFECTS: A BRIEF REVIEW
A visual field defect that presents as an area in which no intensity of light can be seen is known as a contraction. An area of partially reduced vision is called a depression. A localized contraction or depression in the central field that is surrounded by a normal field of vision is known as a scotoma.
A field defect in one eye suggests a possible lesion anterior to the optic chiasm. Lesions of the retina and optic nerve cause monocular defects. Selective damage to the nerve fiber bundles can result in arcuate or altitudinal field defects.
Binocular defects may originate from the optic chiasm, optic tracts, optic radiations, or visual cortex. Because of the crossing of the nerve fibers at the optic chiasm, lesions at this location produce bitemporal hemianopsias. This type of defect has no congruity (that is, similarity between binocular visual field defects). Congruity, or similarity, increases the farther back in the visual pathway a lesion occurs. Optic tract lesions result in homonymous hemianopic defects that are incongruous. Lesions in the optic radiations and visual cortex also form homonymous hemianopic or quadrantanopic defects, but these are much more congruous.
In many cases, the density or severity of visual field loss reflects its cause. A vascular cause, such as a stroke, causes an extremely dense defect. Slow-growing tumors, on the other hand, produce less severe defects initially.
VISUAL FIELD TESTING
All visual field testing measures the extent of a patient's central and peripheral visual field and any limits of the visual space. The normal visual field extends more than 90° temporally, 60° nasally and superiorly, and about 70° inferiorly. Visual sensitivity is greatest at the fovea (center of the macula); it decreases toward the periphery.
A confrontation visual field test is a simple evaluation that can be performed in the office or at the bedside (Box). In an automated visual field test, each eye is tested separately. Lights of various size and intensity appear within the perimeter while the patient fixates on a central target. The patient signals, usually with a handheld device, each time he or she sees a light. These responses are recorded by computer, and the results are printed out at the conclusion of the testing.
Automated visual field perimeters typically use a grayscale format that shows any defects as darkened areas. Black represents severe visual loss; gray represents moderate visual loss or depression. This representation provides an immediate idea of the size and severity of the defects. The numeric grids give the threshold in decibels for all points checked, which helps quantify the depth of the defect.
Temporal Arteritis
A 69-year-old man had had severe headaches for 3 months. Preliminary bloodwork and neuroimaging (MRI, magnetic resonance angiography) failed to establish a definitive diagnosis. Shortly afterward, he experienced severe vision loss in his left eye. A temporal artery biopsy confirmed a diagnosis of temporal arteritis. Oral prednisone, 80 mg/d, relieved the headaches, but the vision loss persisted. The patient described the remaining vision in his left eye as a central "slit" of vision.

At an examination 2 months after the prednisone was started, the patient's best corrected visual acuity was 20/20 in the right eye and 20/30 in the left eye. The patient had to move his head around to find the slit of vision with his left eye. A prominent afferent pupillary defect was noted in this eye. The slitlamp examination revealed early lenticular nuclear sclerosis in both eyes. The fundus examination findings were normal in the right eye; however, the left optic nerve head was pale (A). This sign of optic atrophy correlates with the afferent pupillary defect. A computerized visual field analysis was normal in the right eye; in the left eye, it showed dense extensive loss except for a small island of vision just off axis to the central point of fixation (B).
Temporal arteritis causes severe vision and visual field loss if untreated. Once vision loss and optic atrophy occur, vision loss is irreversible even with treatment.



Right Inferior Homonymous Quadrantopsia
A 64-year-old man was referred by his optometrist after a screening visual field test identified bilateral right lower field defects. The patient had not noticed any vision deficits.
The patient had undergone a below-the-knee amputation of the right leg after a farming accident 20 years earlier. He recalled that he had taken high doses of morphine for 25 days postoperatively and that vision loss had developed in his superior left visual field. The patient believed that the vision loss was transient.
The patient had diet-controlled diabetes and well-controlled hypertension. His medications included lisinopril, 5 mg/d, and aspirin, 81 mg/d.
On examination, the patient's best corrected visual acuity was 20/20 in each eye. No afferent pupillary defect was noted. Intraocular pressures were elevated at 28 mm Hg in the right eye and 30 mm Hg in the left eye. On gonioscopic evaluation, the anterior chamber angles were open to the ciliary body. Slitlamp examination revealed mild lenticular nuclear sclerosis. A dilated fundus examination showed evidence of cup-to-disc asymmetry with temporal sloping of both optic nerve heads (A and B). A computerized visual field analysis identified a dense right inferior homonymous quadrantopsia and a Bjerrum scotoma (arcuate nerve fiber bundle defect with breakthrough to the blind spot) inferotemporally in the left eye (C and D). A small scotoma was also present in the supratemporal quadrant of the left eye (C).
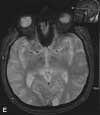
An MRI scan of the brain showed a focal low-signal area on T1-weighted images in the left occipital lobe in the area of the optic radiations. This area became uniformly more hyperintense in signal on T2-weighted images (E). No enhancement was seen after gadolinium-contrast dye injection or on diffusion-weighted imaging (F). These findings were consistent with an old left occipital ischemic infarction, which caused the right homonymous quadrantopsia. The infarction may have resulted from ischemia following blood loss during the farming accident, or it may have occurred during the protracted recovery period. Interestingly, the patient's recollection was that the vision loss had occurred in the superior left visual field and that he had recovered his vision completely.
The visual field findings of a Bjerrum scotoma and an isolated superior scotoma in the left eye in the presence of elevated intraocular pressure and significant optic nerve cupping helped make an additional diagnosis of open-angle glaucoma. Treatment with dorzolamide hydrochloride/timolol maleate solution twice a day in both eyes was begun. One month later, the patient's intraocular pressures had decreased to 18 mm Hg in the right eye and 20 mm Hg in the left eye. The pressures are being monitored every 4 months.


Normotensive Glaucoma
A routine eye examination revealed cup-to-disc asymmetry in the eyes of an 81-year-old man whose intraocular pressures were 15 mm Hg in the right eye and 18 mm Hg in the left eye. His best corrected visual acuity was 20/30 in the right eye and 20/25 in the left eye. He was pseudophakic and had a history of a mild macular pucker in the right eye, which explained the slightly worse vision in that eye.
The cup-to-disc ratio in the right eye was 0.30; in the left eye, it was 0.45 with infratemporal sloping (A and B). Computerized visual field testing revealed a mild infranasal depression in the right eye and a Bjerrum scotoma breaking through to the blind spot inferiorly in the left eye (C and D). A Bjerrum scotoma follows the retinal nerve fiber pattern and takes an arched form around fixation from the blind spot to the horizontal raphe in the nasal field, where it typically ends in a sharply demarcated horizontal or nasal step. These types of defects are often seen in patients who have glaucoma.
Normotensive glaucoma was diagnosed. Because of the patient's optic nerve changes and visual field defects, treatment with a topical antiglaucoma medication was begun in both eyes.
