- Clinical Technology
- Adult Immunization
- Hepatology
- Pediatric Immunization
- Screening
- Psychiatry
- Allergy
- Women's Health
- Cardiology
- Pediatrics
- Dermatology
- Endocrinology
- Pain Management
- Gastroenterology
- Infectious Disease
- Obesity Medicine
- Rheumatology
- Nephrology
- Neurology
- Pulmonology
Takotsubo Cardiomyopathy in a Man With a Gunshot Wound
A 48-year-old African American man with no significant medical history sustained a gunshot wound to the face and shoulder.
A 48-year-old African American man with no significant medical history sustained a gunshot wound to the face and shoulder. He suffered multiple vascular insults, including transection of the proximal right facial artery, intimal injury of the proximal right internal carotid artery, and traumatic false aneurysm of the right proximal external carotid artery. The vascular surgery team repaired the external carotid artery via coiled embolization of the aneurysm and a VIABAHN stent graft endoprosthesis. Arterial spasms occurred 10 minutes after the procedure and were treated with intravenous nitroglycerin. CT scan of the chest showed no infiltrate, masses, pleural effusion, or pneumothorax. The patient was transferred to the surgical intensive care (SICU).
During his SICU stay, the patient was treated with sedatives, pain medications, and standard gastrointestinal and deep venous thrombosis prophylaxis. He also received 2 units of packed red blood cells on hospital day 1 when his hematocrit fell to 21. No pressors were administered during his hospital stay, and he was extubated on day 6.
On hospital day 7, the patient experienced chest pain and dyspnea of sudden onset; oxygen saturation fell to 78% on a 100% nonrebreather facemask. Blood pressure was 142/88 mm Hg; heart rate was regular at 96 beats per minute; respiration rate was 26 breaths per minute. The cardiac examination was normal, with no murmur appreciated. Coarse crackles were heard at the lung bases. There were no other remarkable physical findings.
The patient was reintubated and placed on mechanical ventilatory support. An electrocardiogram revealed sinus rhythm with acute ST elevations in leads V3-V6, I, and AVL. A chest film showed bilateral small pleural effusions that had not been present initially. Bedside echocardiogram showed akinesis of the apex and the mid portions of the anterior and lateral walls; the ejection fraction (EF) was 35% to 40%. Chest CT angiogram was negative for pulmonary embolism. The troponin I level was 26 ng/mL; it later peaked at 33.6 ng/mL.
The patient was treated medically for a presumed ST elevation MI with a heparin drip, aspirin, clopidogrel, an ACE inhibitor, a beta blocker, and a statin.
By hospital day 11, the patient had improved and was extubated successfully. The troponin level trended downward, and the ECG showed normal sinus rhythm with voltage criteria for LV hypertrophy and nonspecific T wave changes. Bedside echo showed an EF of 35% to 0%.
Cardiac catherization on hospital day 15 revealed normal coronary arteries (Figure 1) with anterobasal and posterobasal hyperkinesis, anterolateral and diaphragmatic hypokinesis, and distal ballooning on ventriculography. Ventriculography revealed global LV depression with EF of 45% (Figures 2, 3).
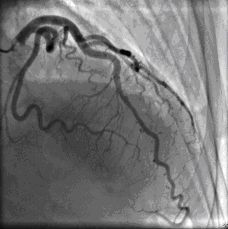
Fig1

Fig2
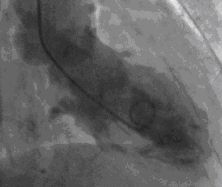
Fig3
The patient was discharged home on hospital day 16 with aspirin (81 mg/d), clopidogrel (75 mg/d), simvastatin (20 mg/d), and metoprolol (25 mg bid). At a 6 week follow-up visit. the patient felt well. A repeat echocardiogram showed a LVEF of 50% without regional wall motion abnormalities.
Discussion
Takotsubo cardiomyopathy, also known as stress induced cardiomyopathy or LV apical ballooning, presents with chest pain, ST elevation that mimics acute MI and congestive heart failure in the setting of normal coronary arteries. We report an unusual presentation of the syndrome here.
Takotsubo cardiomyopathy is a form of reversible heart failure first reported in Japan in the late twentieth century and subsequently described worldwide.1-4 It usually occurs in postmenopausal women experiencing stressful life events, such as the death of a spouse. The clinical presentation is similar to acute MI, with chest pain, dyspnea, and ECG changes.
This case is unique in that the major stressor was a gunshot wound. . During the hospitalization, the patient experienced acute chest pain and dyspnea with dramatic ECG changes. Based on the findings of transient LV dysfunction involving the mid and apical portions of the ventricle without stenotic lesions on coronary angiography, we believe that the diagnosis of Takotsubo cardiomyopathy is applicable.
A diagnosis of Takotsubo cardiomyopathy is always challenging and should be routinely considered in the differential diagnosis of acute MI. Proposed Mayo Clinic criteria5 for Takotsubo cardiomyopathy include
1.Transient hypokinesis, akinesis, or dyskinesis of the LV mid segments, with or without apical involvement; regional wall motion abnormalities extending beyond a single epicardial vascular distribution
2. A stressful trigger-(often but not always present).
3.The absence of obstructive coronary disease or angiographic evidence of acute plaque rupture.
4.New ECG abnormalities (either ST-segment elevation and/or T-wave inversion) or modest elevation in cardiac troponin.
5.The absence of pheochromocytoma or myocarditis.
Our patient’s troponin level was somewhat higher than the range described in the literature and may reflect another unique feature of this presentation.
Several etiological mechanisms for Takotsubo cardiomyopathy have been proposed. In particular, the role of catecholamine-induced myocardial stunning has been suggested secondary to severe emotional and physical triggers, with elevated norepinephrine levels. Ueyama and colleagues3,4 demonstrated a Takotsubo-like cardiomyopathy in a rat immobilization stress model with the apical ballooning prevented by the administration of combined alpha and beta adrenoreceptor antagonists.Others have proposed ischemia-mediated stunning secondary to multivessel epicardial or microvascular spasm.5 Both of these mechanisms (catecholamine stress and vascular spasm) were likely present in our patient.
Approximately 90% of all reported cases have been in postmenopausal women, and the mean age has ranged from 62 to 74 years.6 The reason for the strong female predominance is unclear. One suggested mechanism involves alterations of endothelial function in response to estrogen insufficiency.5
Treatment is focused on supportive care for ongoing signs and symptoms of the acute illness. Hemodynamic and telemetry monitoring is important because these patients are at high risk for arrhythmias from QT prolongation. Prophylactic antiarrhythmic treatment is not recommended; magnesium replacement is suggested in the event of ventricular arrhythmias. The prognosis is quite favorable. Mortality is low and complete recovery is seen in almost all patients within 4 to 8 weeks. Overall, the long-term survival is similar to that of an age-matched general population.5
We urge clinicians to consider Takotsubo cardiomyopathy in the differential diagnosis of acute MI-especially in the context of significant emotional and physical stress and vascular instability.
Figure 1-Cardiac catherization on hospital day 15 revealed normal coronary arteries.
Figure 2-Ventriculography revealed global LV depression with EF of 45%. This is the end diastolic frame of the left ventriculogram.
Figure 3-The end systolic frame of left ventriculogram shows basal contraction with distal ballooning
References:
REFERENCES:
1.
Akashi YJ, Goldstein DS, Barbaro G, Ueyama T. Takotsubo cardiomyopathy: a new form of acute, reversible heart failure.
Circulation.
2008;118:2754-2762.
2.
Kassim TA, Clarke DD, Mai VQ, et al. Cathecolamine- induced cardiomyopathy.
Endocr Pract.
2008;14:1137-1149.
3.
Ueyama T, Kasamatsu K, Hano T, et al. Emotional stress induces transient left ventricular hypocontraction in the rat via activation of cardiac adrenoceptors: a possible animal model of ‘tako-tsubo’ cardiomyopathy.
Circ J.
2002,66:712-713.
4.
Ueyama T, Senba E, Kasamatsu K, et al. Molecular mechanism of emotional stress-induced and catecholamine-induced heart attack.
J Cardiovasc Pharmacol.
2003;41(Suppl 1):S115-S118.
5.
Prasad A, Lerman A, Rihal CS. Apical ballooning syndrome (Tako-Tsubo or stress cardiomyopathy): a mimic of acute myocardial infarction.
Am Heart J.
2008,155:408-417.
6.
Bybee KA, Kara T, Prasad A, Lerman A, et al. Systematic review: transient left ventricular apical ballooning: a syndrome that mimics ST-segment elevation myocardial infarction.
Ann Intern Med.
2004,141:858-865.
