- Clinical Technology
- Adult Immunization
- Hepatology
- Pediatric Immunization
- Screening
- Psychiatry
- Allergy
- Women's Health
- Cardiology
- Pediatrics
- Dermatology
- Endocrinology
- Pain Management
- Gastroenterology
- Infectious Disease
- Obesity Medicine
- Rheumatology
- Nephrology
- Neurology
- Pulmonology
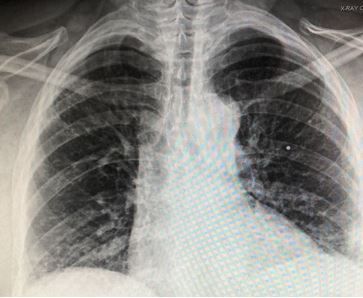
Seen in the ED: Pleuritic Back Pain in a Middle-Aged Woman
History of present illness: A woman in her mid-50’s with a history of rheumatoid arthritis presents to the hospital for 3 days of pleuritic left upper back pain without fever, shortness of breath, chest pain or cough. She also denies any injury and has not had this pain previously.
Vital signs & physical examination. Vital signs are normal except for a pulse oxygen level of 94% on room air. Physical exam is otherwise normal except for bilateral rales heard only with deep breathing.
Relevant test results
Laboratory studies: C-reative protein elevated at 25 mg/L; D-dimer elevated at 1600 mg/L FEU; CBC normal
Imaging: Chest x-ray, image below
What is the most likely diagnosis?
Related Content
