- CDC
- Heart Failure
- Cardiovascular Clinical Consult
- Adult Immunization
- Hepatic Disease
- Rare Disorders
- Pediatric Immunization
- Implementing The Topcon Ocular Telehealth Platform
- Weight Management
- Screening
- Monkeypox
- Guidelines
- Men's Health
- Psychiatry
- Allergy
- Nutrition
- Women's Health
- Cardiology
- Substance Use
- Pediatrics
- Kidney Disease
- Genetics
- Complimentary & Alternative Medicine
- Dermatology
- Endocrinology
- Oral Medicine
- Otorhinolaryngologic Diseases
- Pain
- Gastrointestinal Disorders
- Geriatrics
- Infection
- Musculoskeletal Disorders
- Obesity
- Rheumatology
- Technology
- Cancer
- Nephrology
- Anemia
- Neurology
- Pulmonology
Recurrent Colon Cancer Presenting With Back Pain and Renal Metastases
Renal metastasis from primary colorectal cancer is very rare; 40% of colon cancer patients will have a recurrence, however, after successful initial therapy.
A 64-year-old man underwent right hemicolectomy for adenocarcinoma of the colon and was found to have stage I colorectal cancer (CRC), according to the American Joint Committee on Cancer staging system. Carcinoembryonic antigen (CEA) level was 2.6 ng/mL (normal, 0.1 to 10.0 ng/mL). The patient was monitored with annual CT scans, colonoscopies, and serial CEA measurements.
The patient presented 4 years later with diffuse low back pain which was managed conservatively for approximately 3 weeks. Para-aortic lymphadenopathy seen on a follow-up MRI of the lumbar spine raised concern. The pain did not respond to conservative measures, and the patient began to experience intermittent hematuria, prompting CT investigation. CT imaging of the abdomen (Figures 1, 2, 3) was significant for a new heterogeneous mass in the inferior pole of the left kidney with new bulky retroperitoneal lymphadenopathy encasing the left renal vein. Multiple pulmonary nodules were seen on chest CT (Figure 4). These results raised the concern for metastasis of the primary cancer. Plasma CEA was elevated (72 ng/mL).
Percutaneous needle biopsies of the renal and pulmonary masses confirmed the presence of metastatic adenocarcinoma of the colon. Palliative chemotherapy with folinic acid, fluorouracil, and oxaliplatin (FOLFOX) was initiated for progressive disease.
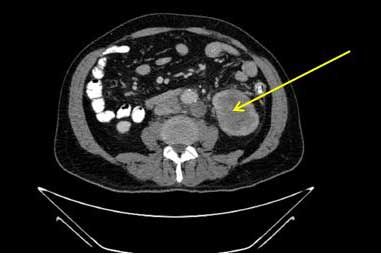
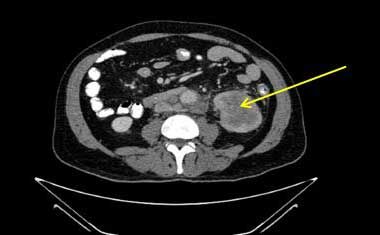
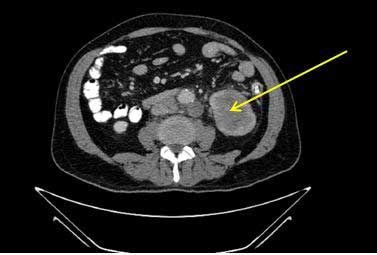
Figures 1-3.
Abdominal CT showing left renal mass (arrows ) with para-aortic lymphadenopathy.

Figure 4.
Chest CT showing multiple pulmonary nodules.
See Discussion on the next page.
Discussion
Renal metastasis from primary CRC is very rare, representing less than 3% of secondary renal neoplasms.1,2 The most frequent primary tumors with renophilic potential are bronchogenic carcinoma followed by breast and GI cancers. Among colon cancer patients, 29% present with metastatic disease and more than 40% of these individuals will have a recurrence after successful initial therapy.
Surgery is the preferred treatment for CRCs. The surgical cure rate for stage I disease approaches 90%, but drops off to 75% and 50% in stage II and III, respectively. In advanced disease, intensive surveillance confers a survival benefit at 5 years. Given the high cure rate for stage I, there is less evidence for postoperative screening.3,4 If curative surgery is not possible, palliative surgery should be performed.4 Use of adjuvant chemotherapy for early-stage disease remains a considerable debate.3 Unless the lesion is resectable, treatment of metastatic CRC is palliative, mainly with systemic chemotherapy. The specific agents used will depend on the primary tumor biology.3 Despite tailored therapy, prognosis remains poor in most circumstances.
Our case was unusual for the renal involvement and more so for the incidental diagnosis of the mass only after the report of pain. The initial MRI was suspicious for unusual nodal disease and together with the subsequent hematuria prompted further evaluation. Back pain in patients with metastatic renal tumors is rarely an exclusive initial symptom. Although other common scenarios might be plausible, metastatic disease should be strongly suspected and investigated in a patient with a recent cancer. Our patient’s rising plasma CEA level also was suggestive of tumor recurrence. Hepatic and peritoneal involvements represent major intra-abdominal sites for spread of CRC. In this case, the renal involvement was confirmed with a tissue biopsy, ruling out possible primary kidney disease.
When back pain is the first symptom of visceral disease, proper diagnosis and treatment may be delayed as conservative measures are pursued. A careful history and physical examination should be obtained especially in patients for whom there is a strong clinical suspicion of cancer or its recurrence. A high index of suspicion for tumor reoccurrence is required when treating those with early-stage colon cancer because detection and treatment can dramatically change the prognosis for the patient if found early.
Take-Home Points
• Metastases of CRC to the kidney are considered rare.
• Low back pain, hematuria, and renal mass can be the initial presentation.
• Disease recurrence should be anticipated within the first 2 to 5 years after cancer diagnosis.
• Rising plasma CEA level postoperatively is suggestive of tumor recurrence or metastases and should prompt further investigation and treatment.
• Surgery is the preferred treatment for early-stage colon cancers and has a high chance of cure.
• Local recurrence or metastatic disease should be expected during postoperative surveillance.
References:1. Weiss L, Grundmann E, Torhorst J, et al. Haematogenous metastatic patterns in colonic carcinoma: an alaysis of 1541 necropsies. J Pathol. 1986;50:195-203.
2. Kobayash H, Mochizuki H, Morita T, et al. Timing of relapse and outcome after curative resection for colorectal cancer: a Japanese multicenter study. Digest Surg. 2006;26:249-255.
3. Kurkjian, C, Murgo AJ, Kummar S. Treatment of recurrent metastatic colon cancer in the age of modern adjuvant therapy. Clin Colorectal Cancer. 2008;7:321-324.
4. Lan YT, Lin JK, Lin TC, et al. Prognostic significance of perioperative change of CEA level in colorectal patients when pre-operative level is normal. Hepatogastroenterology. 2013;59:717-720.
Man With Newly Diagnosed Type 2 Diabetes: What HbA1c Goal-And How to Get There?
May 8th 2013The patient, an active 49-year-old man, had an HbA1c of 8.6 after diabetes was first diagnosed. It’s now 7.6 with metformin and lifestyle measures. Is the current A1c goal adequate, or should you treat more aggressively?
