- Clinical Technology
- Adult Immunization
- Hepatology
- Pediatric Immunization
- Screening
- Psychiatry
- Allergy
- Women's Health
- Cardiology
- Pediatrics
- Dermatology
- Endocrinology
- Pain Management
- Gastroenterology
- Infectious Disease
- Obesity Medicine
- Rheumatology
- Nephrology
- Neurology
- Pulmonology
Prophylactic LAA Closure for Stroke Prevention in AF: Is it Really As Good An Idea As We Thought?
Results of the largest study to assess impact of left atrial appendage closure during routine non-AF-related cardiac surgery raise a few new questions.
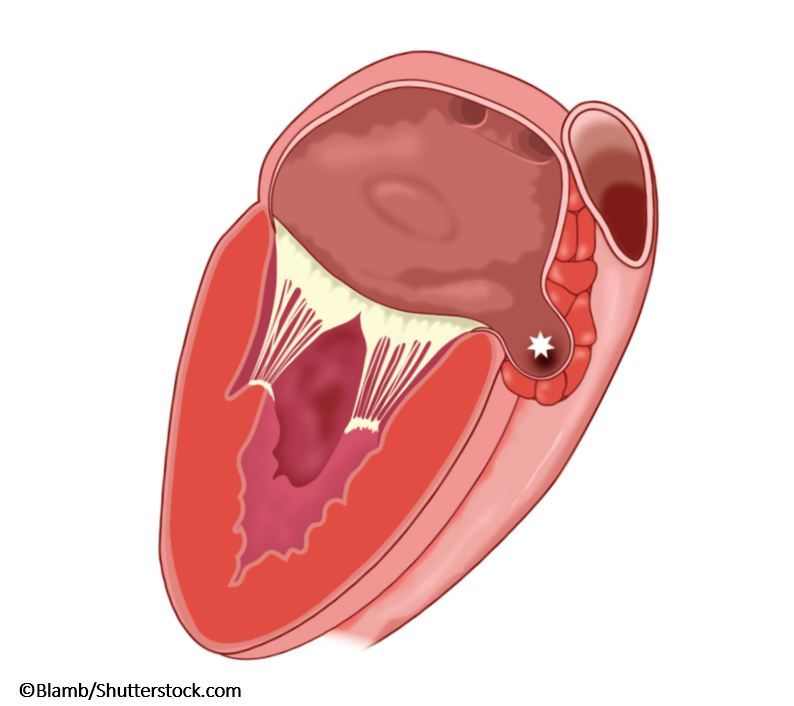
Ischemic stroke and thromboembolism are feared complications of atrial fibrillation (AF), the most prevalent arrhythmia worldwide. In recent years, isolation of the left atrial appendage (LAA)-either through percutaneous placement of an endovascular device, (eg, Watchman) or surgically, with LAA closure. However, as we learn more about the function of the LAA, we are realizing that occlusion of the vessel may actually have hemodynamic and hormonal consequences.
The LAA is the most compliant part of the left atrium. Therefore, occlusion may actually increase left atrial pressure and promote endothelial dysfunction with a paradoxical increase in incidence of AF. This was tested in a prospective observational study of the Mayo Clinic Cardiovascular Surgery Database of 10,633 patients undergoing CABG and/or valve surgery with propensity-matching analysis using 28 covariates; the aim was to estimate the relationship between prophylactic LAA closure and early postoperative AF (POAF [AF ≤30 days of surgery]), ischemic stroke, and mortality.
Surprisingly, the incidence of POAF was 3.88X (95% CO 2.89-5.20) (~69% vs 39%) higher in patients with LAA closure (through ligation or excision) even after adjusting for all covariates. However, this did not translate into adverse clinical outcomes, at least in the short term, and there was no significant increase in the risk of stroke (adjusted HR 1.07, 95% CI 0.72-1.58) or mortality (adjusted HR 0.92, 95% CI 0.75-1.13) during median follow-up of 9.1 years. LAA closure did not add to surgical complications.
As both surgical and percutaneous LAA occlusion become increasingly popular, results from large studies like this one, with long follow-ups will help answer the important question of whether the practice should become routine. In this particular study, the rate of POAF increased with LAA closure, suggesting that inflammation and possibly worsening diastolic dysfunction may well be the underlying mechanism explaining these findings.
So, what will you be telling the surgeons the next time you send a patient for CABG or valve surgery? Do you ask them to close the appendage?
Source: Rowlens M. Melduni RM, Schaff HV, Lee H-C, et al. Impact of left atrial appendage closure during cardiac surgery on the occurrence of early postoperative atrial fibrillation, stroke, and mortality: a propensity score-matched analysis of 10 633 patients. Circulation. 2017;135:366-378. doi: 10.1161/CIRCULATIONAHA.116.021952. Epub 2016 Nov 30.
