- Clinical Technology
- Adult Immunization
- Hepatology
- Pediatric Immunization
- Screening
- Psychiatry
- Allergy
- Women's Health
- Cardiology
- Pediatrics
- Dermatology
- Endocrinology
- Pain Management
- Gastroenterology
- Infectious Disease
- Obesity Medicine
- Rheumatology
- Nephrology
- Neurology
- Pulmonology
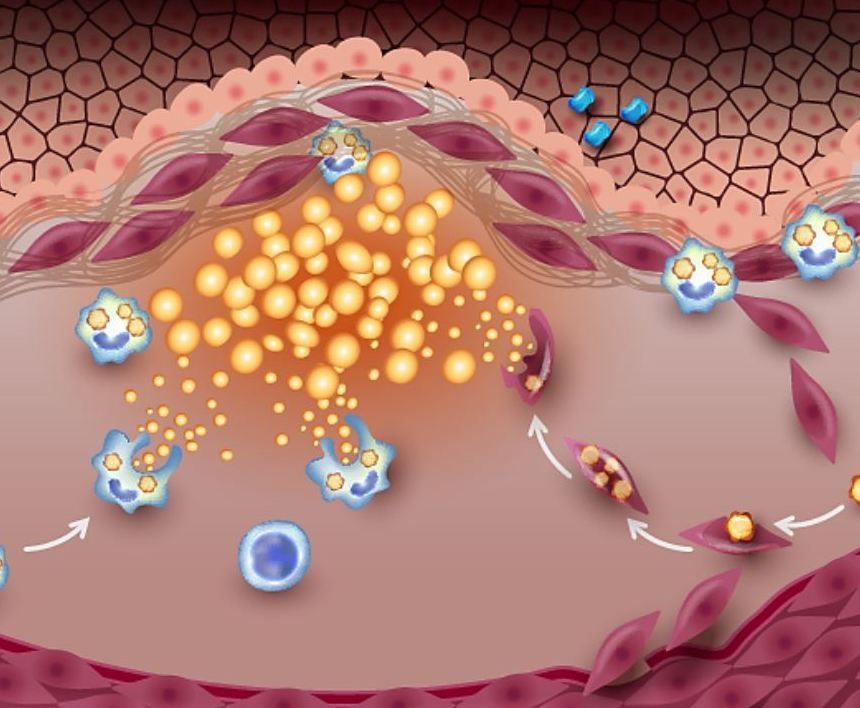
Progression of Subclinical Atherosclerosis Independently Predicts All-Cause Mortality
The use of visual imaging to detect atherosclerosis at its earliest stages and to quantify the burden enhances predictive value of traditional risk assessment tools.
Subclinical atherosclerotic plaque burden and plaque progression were each independently associated with the risk of all-cause mortality in a population of asymptomatic adults without a history of clinical cardiovascular disease (CVD), according to results of a study published in the Journal of the American College of Cardiology that used a combination of noninvasive methods to quantify plaque burden.1
©Tefi/stock.adobe.com
For the study, 5716 adults were examined by vascular ultrasound (VUS) to quantify carotid plaque burden (cPB) and by computed tomography to calculate a coronary artery calcium (CAC) score. Follow-up carotid VUS was performed a median of 8.9 years following the baseline examination. According to the authors, the study was the first to show the research value of 3D echocardiography among other advanced imaging technology to detect large vessel atherosclerotic disease in advance of symptomatology.
"The long asymptomatic phase of the disease presents a window of opportunity that has not been exploited in the younger population," lead author Valentin Fuster, MD, PhD, president, Mount Sinai Fuster Heart Hospital and general director, Centro Nacional de Investigaciones Cardiovasculares Carlos III (CNIC), said in a CNIC statement.2
Currently available CVD risk prediction tools are based on conventional CV risk factors (CVRFs) which are useful for population estimates of risk but have limited accuracy for individuals or for long-term risk prediction, Fuster and colleagues wrote.1 Noninvasive vascular imaging, including VUS and CT-detected CAC, is used increasingly to enhance CV risk assessment. Assessing the extent or burden of subclinical atherosclerosis, beyond its presence, using both technologies, can further refine risk classification, they continued. However, findings of existing research are inconsistent and there is very little data to support the predictive value, independent of traditional CVRFs, of VUS-detected subclinical cPB and its progression and all-cause mortality. The current study was designed to fill the data gap.1
Between January 2008 and June 2009, the prospective BioImage study enrolled 7687 asymptomatic members of a large national health system. The full study population was assessed by carotid VUS and CAC scoring—732 participants underwent a second, follow-up carotid VUS approximately 9 years after the baseline exam. Participants were followed until October 2021 for the primary outcome, all-cause mortality.1
FINDINGS
The final cohort had a mean age of 68.9 years, and just more than half (56.7%) were women. At baseline, 87.7% of participants had subclinical atherosclerosis; 57.6% had multiterritorial disease (some cPB in 1 or both carotids and CAC score >0), 19.7% had disease only in the carotids, and 10.5% had only CAC, according to the study.
Fuster et al reported after a median follow-up of 12.4 years there were 901 (16%) deaths. After they adjusted models for CVRFs and for participants’ medication, the baseline cPB measure and CAC score were both significantly associated with all-cause mortality (fully adjusted trend HR 1.23, 95% CI 1.16-1.3,2 and HR 1.15, 95% CI 1.08-1.23), respectively (both P <.001), providing evidence of the added prognostic value of both measures. Overall, however, cPB contribution was the stronger of the 2, authors noted.1
Among the subgroup of 732 participants with a follow-up carotid VUS nearly 9 years after baseline imaging, the median cPB progressed from 29.2 mm3 to 91.3 mm.3 Investigators identified a significant association between cPB progression and all-cause mortality, which remained after adjusting for cardiovascular risk factors and baseline cPB (HR 1.03, 95% CI 1.01–1.04 per absolute 10-mm3 change; P =.01).1
“[VUS] is a noninvasive and affordable test, and the valuable prognostic information it provides can be used to improve risk stratification and to target lifestyle recommendations for the control of cardiovascular risk factors,” Borja Ibáñez, MD, PhD, scientific director at CNIC and a cardiologist at Fundación Jiménez Díaz, concluded in a statement.2
References
