Primary Care Reluctance to Treat Addiction Linked to Poor Institutional Support: New Study
Among GPs, IMs, FPs, the primary reason for reluctance to treat addiction is lack of support in the "institutional environment," followed by concerns over personal skills.
A study surveying 60 years of research on addiction has distilled the primary barriers to physician engagement with addiction in clinical practice. The leading one, cited in 81% of the studies reviewed was “institutional environment,” a term that encompasses factors including lack of institutional support for addiction treatment; insufficient resources, eg, staffing and training; challenges in organizational culture; and competing demands on time.1
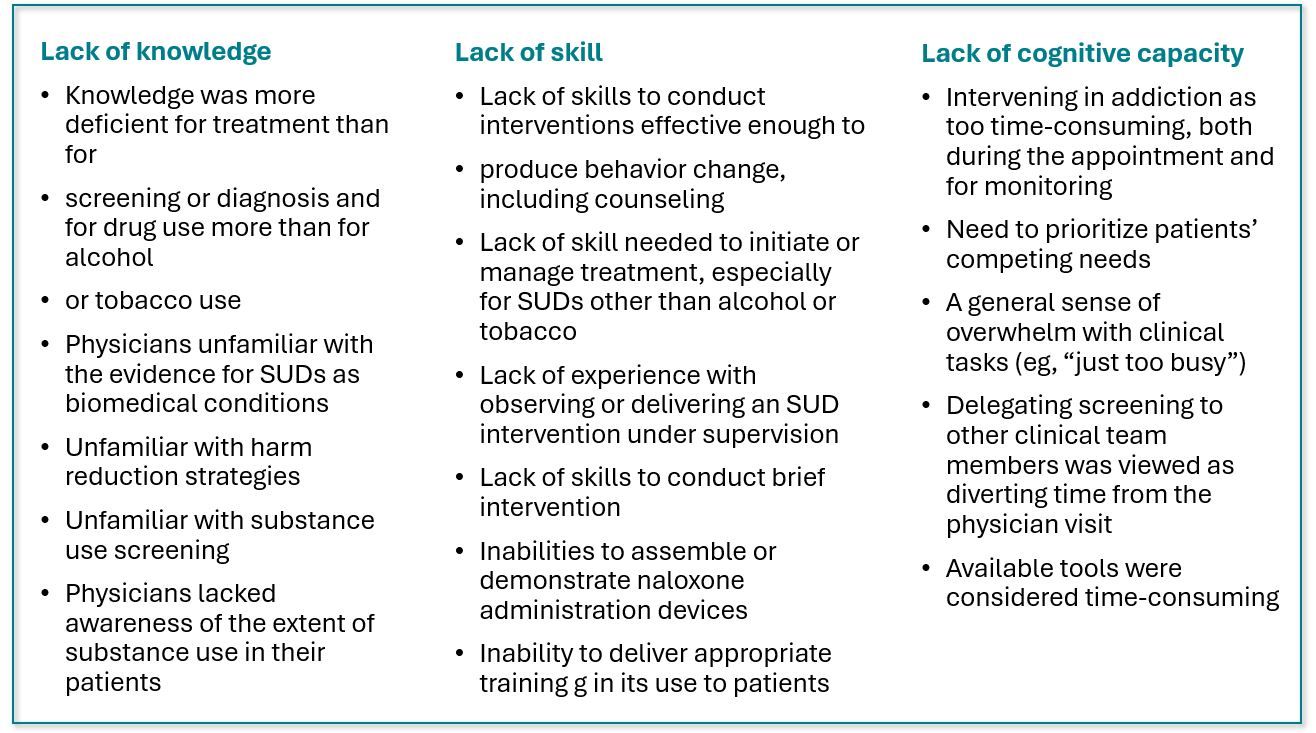
The collection of environmental factors was followed by more personal and/or professional reasons for the reluctance, including insufficient skill (74%), lack of cognitive capacity to manage a certain level of care (74%), and inadequate knowledge (72%), senior study author Wilson S Compton, MD, deputy director of the National Institute on Drug Abuse (NIDA), and colleagues reported.1
©Minerva Studio/stock.adobe.com

Lack of knowledge and lack of skill were most frequently paired reasons for reluctance to intervene (61.1%) followed by the combination of cognitive capacity and institutional environment (60%).
Negative social influences as barriers figured prominently in 65.8% of the studies and were defined as beliefs about public and community acceptance of addiction care. More than half the studies (56%) revealed fear of harming or losing the patient-physician relationship (eg, causing offense or provoking avoidance) as deterrents for intervening in addiction, Compton and team wrote.1
“People with substance use disorders must be able to access compassionate and evidence-based care at any touchpoint they have with a health care provider,” National Institute on Drug Abuse (NIDA) Director Nora D Volkow, MD, said in a NIDA news release. “To make that vision a reality, clinicians across all medical disciplines need greater training, resources, and support in caring for people with addiction, so that they feel prepared to proactively offer prevention, screening, treatment, harm reduction, and other tools that can help save lives.”
Although there is a wide variety of evidence-based practices (EBP) including medications available to treat alcohol and drug use disorders and efforts are ongoing to train and support clinicians to implement them, uptake and adoption have been low, study authors state.1 The lack of engagement with resources is all the more frustrating given that overdose is the country’s leading cause of injury-related mortality, with nearly 108 000 overdose-related deaths reported in 2022. Annual deaths related to alcohol exceeded 140 000 from 2015 to 2019, according to the study.1
Demand high, resources low
For the services that are available, the demand now far exceeds capacity. In 2022, nearly 49 million Americans had at least one substance use disorder but just one-quarter of them were able to receive treatment in the past year, according to NIDA. Fewer than half the 9 million adults who needed treatment for opioid use disorder (OUD) in 2022 received any type and only one-quarter received medication for OUD.1
Furthermore, even screening for substance use disorders is low, “creating missed opportunities to intervene in harmful substance use or recognize and discuss potential progression to a severe disorder,” researchers observed.
Compton and the NIDA team retrieved data from studies spanning the years 1960 to 2021 that included feedback from 66 732 clinicians, primarily in general practice and internal and family medicine and in office settings. Of the 4 general categories of addiction interventions clinicians expressed reluctance about, treatment was addressed most often, followed by screening and assessment. Harm reduction and recovery support were discussed least often, according to the study.
“People with substance use disorders must be able to access compassionate and evidence-based care at any touchpoint they have with a health care provider."
NIDA Director Nora D Volkow, MD
NIDA Director Nora D Volkow, MD
The substances most often studied alone were opioids (104 studies), alcohol (86 studies), and nicotine (30 studies). In studies that reported on multiple drugs, alcohol was included most often.1
They authors noted that nearly all of the studies (97.3%) were published in or after 2000, reflecting the growing interest in the field as well as the rapid evolution of treatment.
Among the safe and effective EBPs to treat substance use disorders and related morbidity and mortality, the authors cite screening, brief intervention, and referral to treatment, as well as behavioral therapies and pharmacotherapies for nicotine, alcohol, and opioid use disorders.
They also suggest several strategies that have potential to assuage clinicians’ feelings about restrictive institutional environments, eg, a greater commitment to making needed workflow and staffing changes as well as investment in in-service training; dismantling barriers between addiction services and medical and mental health care; and working with payers to provide reimbursement that covers the actual cost of addiction services.1
Among the study limitations the authors acknowledged are the inconsistent use of terminology across studies, study design without benefit of a theoretical framework, and the ever-fluid nature of drug development, drug policy, and regulations, making comparisons across decades a challenge.1
“Developing new addiction treatments is crucial, but it is equally important to rigorously study how to implement these treatments so that they make it into the doctor’s office and reach the people who need them,” Compton said. “Survey results have helped us better understand the treatment landscape, so the next step is to test ways to change behavior and attitudes around providing addiction treatment, in order to break down barriers to the addiction care that people seek.”
Examples of clinician reasons for reluctance related to knowledge, skills