- Clinical Technology
- Adult Immunization
- Hepatology
- Pediatric Immunization
- Screening
- Psychiatry
- Allergy
- Women's Health
- Cardiology
- Pediatrics
- Dermatology
- Endocrinology
- Pain Management
- Gastroenterology
- Infectious Disease
- Obesity Medicine
- Rheumatology
- Nephrology
- Neurology
- Pulmonology
Post-CABG AF: Not So Benign
Post-procedure AF, once thought to be an artifact of healing, turns out to be a sign of significant risk, a new study finds.
Copyright hywards/Shutterstock.com
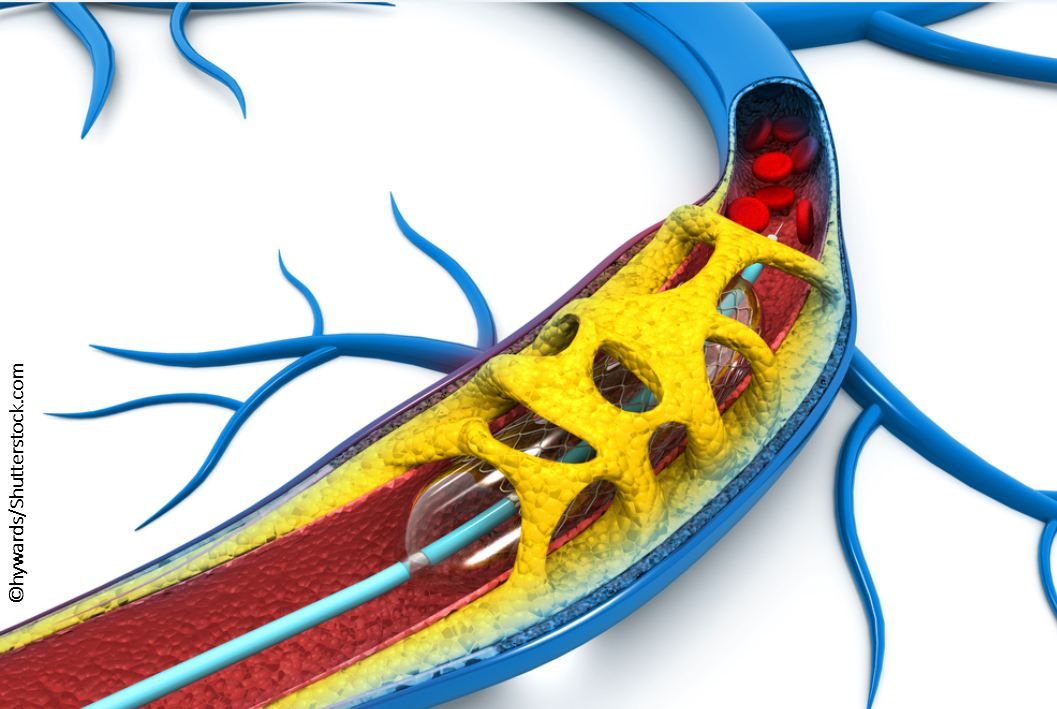
By far, the most common reason for a cardiology consultation for a patient following CABG surgery is postoperative atrial fibrillation (AF). The increased risk of AF after CABG may be the result of a number of post-surgical stressors, not least of which are pericardial and atrial inflammation, including myocyte edema; electrolyte and fluid shifts; and heightened catecholamine states. It would be reasonable to expect these types of triggers to be attenuated following PCI, which is less likely to cause many of the hemodynamic and hormonal stressors of CABG. I get these consults regularly, but I am not sure I ever stopped to consider the short- and long-term prognosis associated with postoperative AF.
As PCI is now becoming an attractive alternative to CABG for left main (LM) disease, the authors of a recent analysis in the Journal of the American College of Cardiology attempted to study the incidence and prognosis of new-onset AF in patients with LM disease who were revascularized with one of these two modalities.
This study reported a post-hoc analysis of the EXCEL trial, which was a randomized controlled trial (RCT) of PCI with everolimus-eluting stent vs CABG in 1905 patients with LM CAD and low to intermediate SYNTAX score (<32). It was not surprising that occurrence of AF was significantly more common in CABG patients (18%) vs PCI patients (0.1%) and for some of the reasons we suspected – essentially all the patients who got new onset AF were CABG, not PCI, patients. Also not a surprise, those who developed AF tended to be older, with higher BMI and lower LV function.
What was surprising was the worse short- and long-term prognosis associated with new onset postoperative AF, even though it was transient in some. In the short term, these patients had increased TIMI major/minor bleeding (due to more anticoagulant use) at 30 days and longer length of stay in the hospital. In the long term, at 3 years, after multivariate adjustment, they had a two- to four-fold higher risk of multiple adverse CV outcomes, including stroke (6.6% vs 2.4%, HR 4.19), death (11.4% vs 4.3%, HR 3.02), and the composite of death/MI/stroke (22% vs 12%, HR 2.13).
So what we once thought was a natural, relatively benign “healing” process of the heart turns out can carry more short- and long-term risk than we have appreciated. This begs the following questions:
1. Should we be more aggressive in preventing AF following CABG (prior strategies studied include beta blockers, amiodarone, botulinum toxin)?
2. When AF is found, should we be more aggressive with anticoagulation and follow these patients more closely (ie, screen more aggressively for recurrence of AF)?
3. Are the underlying factors driving the risk more than AF itself (is AF more of a marker of risk)?
4. Are we underutilizing oral anticoagulants (only ~10% of patients in the present study were discharged on oral anticoagulants)?
Although RCTs are needed to definitively answer some of these question, for the time being, the answer to all of them appears to be a resounding “Yes.”
So, the next time you get a “straightforward” postoperative AF-after-CABG consult…beware… there is more risk here than meets the eye and just getting them through the “AF” period may not be enough.
Source: Kosmidou J, Chen S, Kappetein AP, et al. New-onset atrial fibrillation after PCI or CABG for left main disease. The EXCEL trial. J Am Coll Cardiol. 2018;71:739-748. DOI:10.1016/j.jacc.2017.12.012
