- Clinical Technology
- Adult Immunization
- Hepatology
- Pediatric Immunization
- Screening
- Psychiatry
- Allergy
- Women's Health
- Cardiology
- Pediatrics
- Dermatology
- Endocrinology
- Pain Management
- Gastroenterology
- Infectious Disease
- Obesity Medicine
- Rheumatology
- Nephrology
- Neurology
- Pulmonology
Pneumonia Significantly Increased Costs of ICU Stays
The price tag for an ICU stay was more than 5 times higher for pneumonia patients. Can we find an ounce of prevention?
Staphylococcus aureus
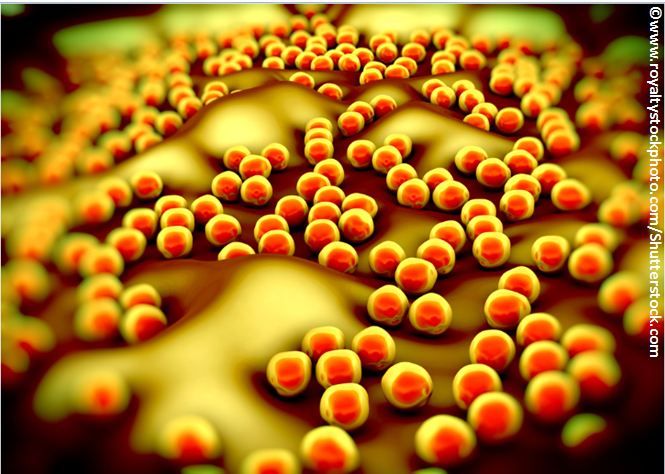
Pneumonias caused by Staphylococcus aureus and Pseudomonas aeruginosa resulted in significantly increased health care utilization and costs among patients in the ICU, according to the results of a retrospective study published in BMC Health Services Research.
Whereas patients in the ICU without pneumonia incurred healthcare costs of about $30,000, those with S aureus or P aeruginosa pneumonia had costs of $150,000 to $213,000, the study found.
“Our findings highlight the comprehensive economic consequences attributed to S aureus and Paeruginosa pneumonia and can permit policy makers, payers, and healthcare providers to assess the effect of prevention or therapeutic efforts on the cost and morbidity of these ICU infections,” wrote Moe H. Kyaw, of MedImmune, and colleagues.
The study used data from a medical and pharmacy claims database that included 29.6 million enrollees. The researchers identified patients in the ICU with S aureus or P aeruginosa pneumonia based on ICD codes and compared these patients with those admitted to the ICU without pneumonia.
Kyaw and colleagues found that those patients with pneumonia had a significantly longer average hospital stay (37.9 days or 55.4 days vs 7.2 days; P<.001) and a significantly longer stay in the ICU (6.9 or 14.8 days vs 1.1 days; P<.001) compared with patients without pneumonia.
Patients with S aureus or P aeruginosa pneumonia also were more likely to have mechanical ventilation (62.6% or 62.3% vs 7.4%; P<.001) and a higher mortality rate (16.0% or 20.2% vs 3.1%; P<.001).
“Mean total costs for the index hospitalization were approximately 4 and 6 times greater in patients with S aureus or P aeruginosa pneumonia, respectively, than in those in the control group, resulting in incremental costs of > $100,000,” the researchers wrote.
Specifically, the researchers calculated inpatient and total costs and found costs of $156,259 and $164,437 in the S aureus pneumonia cohort and $226,631 and $235,381 in the P aeruginosa pneumonia cohort compared with $38,765 and $44,427 for the control cohort.
“Overall, these results indicate that S aureus and P aeruginosa pneumonia in ICU patients impose substantial costs, healthcare utilization, and burden for patients,” the researchers wrote. “Our results highlight the economic importance of effective interventions to reduce the burden of S aureus and P aeruginosa pneumonia in ICUs in the United States.”
References:
Kyaw MH, Kern DM, Zhou S, et al. Healthcare utilization and costs associated with S. aureus and P. aeruginosa pneumonia in the intensive care unit: a retrospective observational cohort study in a US claims database.BMC Health Services Research. 2015;15:241.
