- Clinical Technology
- Adult Immunization
- Hepatology
- Pediatric Immunization
- Screening
- Psychiatry
- Allergy
- Women's Health
- Cardiology
- Pediatrics
- Dermatology
- Endocrinology
- Pain Management
- Gastroenterology
- Infectious Disease
- Obesity Medicine
- Rheumatology
- Nephrology
- Neurology
- Pulmonology
Perimenopause Misdiagnosis Affects Nearly 40% of Women as Clinicians Fail to Recognize Hormonal Transition
Nearly 40% of perimenopausal women report misdiagnosis as clinicians treat for anxiety and depression without addressing underlying hormonal imbalance.
Findings from a new national survey of more than 1,000 women has revealed that 39% felt they were misdiagnosed when seeking care for perimenopause symptoms, exposing a healthcare system that routinely treats mental health conditions without addressing underlying hormonal changes.1
©Olivier Le Moal/stock.adobe.com

The 2025 "Perimenopause Focus" survey, commissioned by health and wellness company Biote and conducted in August 2025, examined US women ages 30 to 60 who work full or part-time. The findings document widespread treatment for mental health conditions during perimenopause: 33% of respondents received diagnoses and treatment for anxiety, 27% for depression, 25% for mood swings, and 13% for panic attacks. Among women prescribed medication for mental health conditions, more than one-third (39%) believed they were not appropriately diagnosed.1
Overlap Complicates Diagnosis
The overlap between symptoms of perimenopause and depression can lead to diagnostic confusion, the survey results showed. Seven of the eight conditions on the Patient Health Questionnaire depression scale (PHQ-8) may actually be caused by perimenopause or menopause rather than clinical depression, including sleep disruptions, changes in appetite, fatigue, trouble concentrating, and mood disturbances.1 The survey authors cite research confirming that women are 1.5 to 2 times more likely to experience depressive symptoms during perimenopause compared to their premenopause years, with those who have no prior mental health history facing 2 to 4 times higher risk of developing depression during this stage.1
Critical treatment gap. The data highlight a critical gap in women's healthcare during a very vulnerable life passage. "We are seeing anxiety and depression being treated as isolated conditions when providers should be addressing the hormonal imbalance at the root of the problem," Bruce Dorr, MD, NP, of Littleton Gynecology and Wellness, in Colorado and Biote senior medical advisor, said in a statement. "Many of these women know something isn't right with their diagnosis, but they don't know where to turn for better care."2
The survey documented that 45% of respondents report perimenopause symptoms have negatively impacted their emotional, social, or mental health, with an additional 21% unsure of the impact. More than one-third (35%) of respondents wished they had known that perimenopause can affect mental health, not just physical well-being.1
Communication Breakdown
Only 37% of women surveyed reported having proactive and satisfactory conversations about perimenopause with their healthcare provider, meaning nearly two-thirds failed to get adequate medical guidance throughout this transition, the authors stressed. The breakdown reveals1:
- 42% said their primary care provider or OB/GYN had initiated discussions about perimenopause symptoms during regular appointments
- 37% reported no conversations at all
- 26% received inadequate or incomplete information
Unsatisfactory conversations. The quality of conversations that do occur often falls short. The survey found that among the 19% of women who spoke with their clinician about perimenopause, many felt their concerns weren't taken seriously or fully addressed. Of respondents unsatisfied with their provider interactions, 65% felt their concerns weren't fully addressed, 26% said their providers did not take their concerns seriously, and 9% were told to speak with someone else about their concerns.1
Millennials vs Gen X. Generational differences were also observed in the data. Among Millennial women ages 30-44, 46% were not proactively asked by their providers if they had experienced perimenopause symptoms, compared to 29% of Gen X women ages 45-60. When it comes to learning about perimenopause from providers, only 18% of Millennials received information from their primary care provider or OB/GYN, compared to 41% of Gen X women.1
©pikovit/stock.adobe.com
Diagnostic Testing Gaps
More than half of women surveyed (52%) reported that their health care professional never suggested a blood test of their hormone levels. Among respondents who did have blood tests, 33% reported no meaningful follow-up discussion with their clinician to interpret the results. This includes 16% who were simply told their results were "normal" with no further discussion, and 17% who received no follow-up communication at all.1
Nearly half (46%) of respondents experiencing perimenopause symptoms reported that their health care professional had never offered any treatment for their symptoms. The Menopause Society recognizes hormone therapy as FDA-approved first-line therapy for symptoms like severe hot flashes,3 yet 41% of women wished they had known that treatment options were available for perimenopause symptoms.1
Dr Google Will See You Now
In the absence of professional guidance, women take research into their own hands, according to the results. Only 15% of respondents felt adequately informed and knowledgeable about perimenopause when symptoms began, or put another way, 85% did not feel informed and knowledgeable about perimenopause early in this stage.1 Women are more likely to learn about perimenopause from more readily available sources than a health care professional. When seeking information, 42% of survey respondents turned to Google and 42% tapped family members, while only 26% recieved information from their primary care provider or OB/GYN. The suvery authors learned that women's self-directed research spans digital platforms, including health and medical websites (37%), social media platforms (29%), and news articles (13%).1
"I Wish I Had Known..."
56% wished they knew symptoms can start earlier than expected
41% wished they knew treatment options were available for perimenopause and associated symptoms
37% wished they knew symptoms can be severe and disruptive
37% wished they knew perimenopause can last for years,
35% wished they had known perimenopause can impact mental health as much as physical health
25% wished they knew how to advocate for themselves with doctors
Medical Education Deficit Drives Provider Gaps
The Perimenopause Focus authors assert that inadequate provider conversations reflect systemic problems in medical training. They cite data revealing that only 31% of OB/GYN residency programs in the US incorporate a menopause curriculum.4 They also point out that there are just 1,300 North American Menopause Society (NAMS)-certified practitioners in the United States, and no standardized menopause education requirements exist for medical students.4
"We've created a system where the onus is on women to search for that rare provider with specialized perimenopause knowledge," Dorr said. "While recent legislative efforts are aiming to improve clinical education, millions of women can't wait for systemic change. They need comprehensive, effective care today."1
Perimenopause is Complex
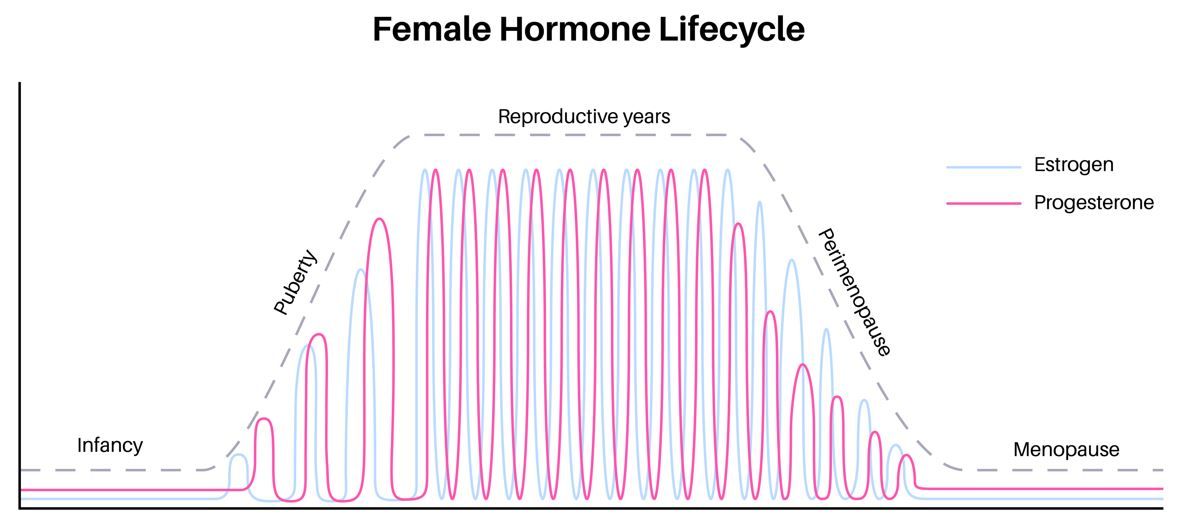
In the United States, menopause occurs at an average age of 51, but perimenopause can begin as early as a decade prior.5 The hormonal shifts in estrogen and progesterone during this transition affect multiple body systems, leading to symptoms including sleep disruptions, cognitive changes, emotional disturbances, physical discomfort, and changes in sexual and reproductive health.5
Multiple studies document the extensive range of perimenopause symptoms. Research analyzing symptom logs has identified up to 45 different symptoms that can result from hormonal imbalances, and each woman's experience is unique.6,7 Studies confirm that symptoms occur in predictable clusters, including mood/cognitive, digestive, and vasomotor groupings, and can vary in intensity and persist for years. Without proper recognition or medical support, perimenopause can disrupt family life, work performance, and emotional well-being, underscoring the urgent need for providers who can recognize and effectively treat the full scope of this transition.6,7
Regulatory Changes May Open Opportunities
Dorr emphasized the timing of the survey alongside the FDA's recent decision to remove the black box warning from hormone therapies. "Nearly 40% of women felt misdiagnosed, and now we know that the very treatments that could have addressed their root hormonal issues carried warnings that scared away both patients and providers," he said in the statement.1 "Having the FDA acknowledge that these warnings were based on outdated science and have done real harm to women's health has created a pivotal moment for women's healthcare. We are committed to ensuring that providers have the education and confidence to offer hormone optimization as a safe, effective treatment option."1
References
- Perimenopause Focus: misunderstood and misdiagnosed, survey reveals hidden crisis. Biote. November 2025. Accessed November 14, 2025. https://biote.com/wp-con
- Nearly 40% of women say they were misdiagnosed during perimenopause, natioanl survey reveals. News release. biote. November 13, 2025. Accessed November 14, 2025. https://ir.biote.com/node/8891/pdftent/uploads/2025/11/Biote-Perimenopause-Survey-Whitepaper.pdf
- NAMS Position Statement. The 2022 hormone therapy position statement of The North American Menopause Society. Menopause. 2022;29(7):767-794. doi:10.1097/GME.0000000000002028
- Allen JT, Laks S, Zahler-Miller C, et al. Needs assessment of menopause education in United States obstetrics and gynecology residency training programs. Menopause. 2023;30(10):1002-1005. doi: 10.1097/GME.0000000000002234
- What is menopause. National Institute on Aging. Last reviewed October 16, 2024. Accessed November 14, 2025. https://www.nia.nih.gov/health/menopause/what-menopause
- Aras SG, Grant AD, Konhilas JP. Clustering of > 145,000 symptom logs reveals distinct pre, peri, and menopausal phenotypes. Sci Rep. 2025;15(640). doi:10.1038/s41598-024-84208-3
- Harlow SD, Karvonen-Gutierrez C, Elliott MR, et al. It is not just menopause: symptom clustering in the Study of Women’s Health Across the Nation. womens midlife health. 2017;3(2). doi:10.1186/s40695-017-0021-y
