- Clinical Technology
- Adult Immunization
- Hepatology
- Pediatric Immunization
- Screening
- Psychiatry
- Allergy
- Women's Health
- Cardiology
- Pediatrics
- Dermatology
- Endocrinology
- Pain Management
- Gastroenterology
- Infectious Disease
- Obesity Medicine
- Rheumatology
- Nephrology
- Neurology
- Pulmonology
OTC Contraception Option Improves Access For Women at High Risk for Unintended Pregnancy
Opill OTC has significantly increased contraceptive use and shifts from less effective options among women who are uninsured, of racial/ethnic minorities, and live in the rural US.
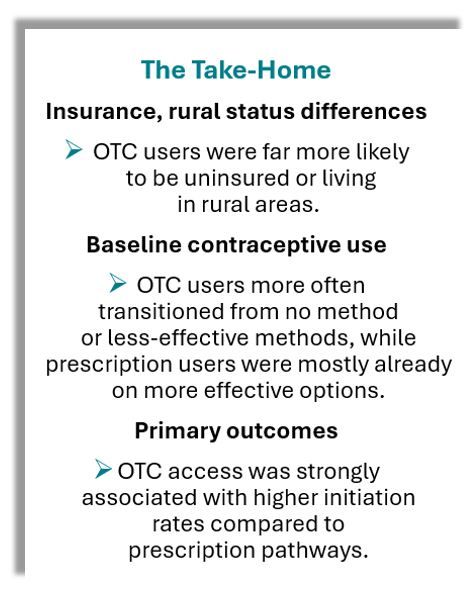
Over-the-counter (OTC) access to oral contraceptives in the US appears to be reaching individuals with the greatest barriers to care, according to findings of a a new national study. Investigators from the Center for Reproductive Health Equity, Oregon Health & Science University, in Portland, OR, reported that individuals using the newly approved OTC progestin-only pill were significantly more likely to initiate contraception after previously using no method or a less-effective method, compared with those accessing pills through prescriptions.
©Windy Night/stock.adobe.com

Rural Dwellers, Uninsured More Likely to Use OTC
In a cohort of 986 individuals of childbearing age (15–45 years), OTC oral contraceptive users accounted for 32.5% of participants. Compared with prescription pill users, OTC users were more often uninsured (31.6% vs 3.5%) and more likely to live in rural areas (14.4% vs 8.4%), according to the study.
The researchers emphasized that the availability of OTC contraception was associated with a 31.8–percentage point greater likelihood of use among participants not previously using contraception and a 41.0–percentage point greater likelihood of transitioning from less-effective method, such as condoms or emergency contraception.
The findings, study authors wrote, "suggest that the OTC OCP may serve as a critical access point for contraceptive initiation and method switching, particularly for populations facing structural barriers to care." The results are "particularly salient in the context of ongoing threats to reproductive health care access under proposed federal and state-level policy changes," they added.
Opill Approved in 2023
The FDA approved the first OTC oral contraceptive pill, a progestin-only formulation (Opill; Perrigo), in 2023. The pill became widely available online and in pharmacies by April 2024. Oral contraceptives are the most common form of reversible contraception in the US, with nearly 80% of reproductive-aged women reporting use at some point (Daniels). Globally, women in more than 100 countries have had access to OTC contraception for more than 5 decades. (Grindlay)
Proponents of OTC availability argue that removing prescription barriers could reduce unintended pregnancy rates by making contraceptives more accessible to populations facing systemic barriers, including adolescents, uninsured individuals, and those living in rural areas. The present study sought to test whether early adoption of OTC oral contraceptives in the US reflected these access goals.
Study Population
For cross-sectional study, investigators drew from baseline data in a national, prospective cohort. Eligible participants were aged 15–45 years, at risk for pregnancy, and obtaining oral contraceptives between April 2024 and February 2025 either by prescription or OTC purchase. Partnering with a national pharmacy chain, the researchers tapped 63 pharmacies across 31 states, the manufacturer’s website, and targeted digital outreach.
Self-administered surveys collected demographic, reproductive, and behavioral information. The research team defined the primary outcomes specifically as 1) initiation of contraception among individuals not using any modern method, and 2) transition from less-effective methods to oral contraceptive use. Multivariable logistic regression was used with adjustment for rurality, age, and importance of avoiding pregnancy.
Key Findings
The largest proportion of participants was aged 20–24 years (34.3%), according to the study. OTC contraceptive users were more likely to be adolescents (14.1% vs 6.5% of prescription users) and to identify as Black (15.6% vs 7.1%) or Hispanic/Latina (16.6% vs 9.5%). They also had lower educational attainment and were more frequently from the Southern US.
When study authors evaluated experience with pregnancy and contraceptive use they found that a greater proportion of OTC users compared to those with a prescription for a contraceptive reported a history of pregnancy (32.5% vs 18.6%) and childbirth (28.4% vs 14.7%). Rates of recent counseling on contraceptive use also was lower among OTC users (38.8% vs 60.4%) and this group was more likely to have not used contraception in the past (26.2% vs 9.2%) or to have relied on condoms (27.2% vs 6.8%).
Applying multivariable models, the researchers found that nearly half of OTC users moved from nonuse (42.4%) or less-effective use (49.2%) to use of the pill, compared with only 10.6% and 8.1% of prescription users, respectively.
The most commonly reported reasons for choosing OTC included convenience, avoidance of scheduling an appointment, and lack of a regular physician.
Among the study's limitations, the authors acknowledged that self-selection into OTC vs prescription pathways may reflect unmeasured differences in health care engagement or contraceptive preferences. In addition, the cross-sectional design limited ability to assess long-term outcomes such as continuation and unintended pregnancy rates. They pointed out, also, that the study data were collected early in the roll-out of the OTC pill, so uptake patterns may evolve with time.
Implications for the Future
The study concluded that OTC oral contraceptives are successfully reaching uninsured individuals, adolescents, and those living in rural areas—groups historically at high risk of unintended pregnancy and maternal morbidity. By reducing reliance on less-effective methods, OTC availability may represent an important tool in advancing reproductive health equity, the authors said.
They emphasized that sustained impact will depend on addressing cost barriers. At present, a 3-month supply of the OTC pill costs approximately $50, and insurance reimbursement is inconsistent. Only a subset of states require Medicaid or commercial insurers to cover OTC contraceptives without a prescription. Policy and implementation efforts to ensure broad coverage will be critical to long-term effectiveness.
“More than half of those using OTC access were not previously using a method or were relying on condoms or emergency contraception,” the authors wrote. “Removing prescription requirements appears to help individuals meet their reproductive goals, particularly among underserved populations.”
Future research will track continuation, adherence, and unintended pregnancy rates as OTC use becomes more established in the US.
