- Clinical Technology
- Adult Immunization
- Hepatology
- Pediatric Immunization
- Screening
- Psychiatry
- Allergy
- Women's Health
- Cardiology
- Pediatrics
- Dermatology
- Endocrinology
- Pain Management
- Gastroenterology
- Infectious Disease
- Obesity Medicine
- Rheumatology
- Nephrology
- Neurology
- Pulmonology
Obese Patients with COVID-19 at Higher Risk for ICU Admission, Longer Stay
ENDO 2021: Patients with severe obesity hospitalized for COVID-19 were twice as likely to require ICU admission vs those with normal BMI, according to new findings.
Obese patients hospitalized with COVID-19 are at significantly greater risk of ICU admission and of longer duration of ICU stay compared to people with a normal body mass index (BMI), according to a study presented virtually at ENDO 2021, the Endocrine Society’s annual meeting.
The study also found that despite an apparent more severe disease course among patients with obesity, the risk of mortality was not higher than among those of normal weight.
“The association between obesity and a more severe clinical course of COVID-19 highlights the vulnerability of this population during the current pandemic and the need for public health efforts to prevent and treat obesity, in the current pandemic and beyond,” said lead researcher Yu Mi Kang, MD, PhD, of Yale New Haven Health in New Haven, Conn, in an Endocrine Society press release.
Obesity is recognized as one of the significant risk factors for severe COVID-19. Kang and colleagues sought to evaluate the association of obesity and other clinical factors with outcomes among obese vs non-obese individuals hospitalized with severe COVID-19.
The researchers analyzed data from 3,268 adult patients hospitalized with PCR-confirmed COVID-19 at 5 hospitals within the Yale New Haven Health System between March and November 2020. Median age was 65 years, 49.4% were women; 30.5% were classified as overweight and 43.2% had obesity.
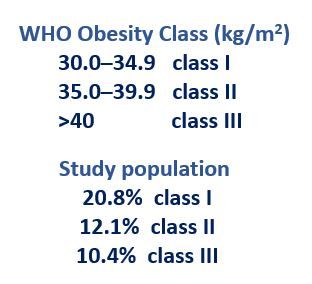
Body mass index (BMI) was calculated using admission weight and height and obesity defined according to world Health Organization classification. The association of obesity and other clinical parameters with mortality were determined using both bivariate and multivariate logistic regression analyses. The multivariate model was adjusted for patient demographics and 8 pertinent comorbid conditions.
Mortality was defined as in-hospital death or transition to hospice care and intensive care use as transfer to intensive care unit (ICU).
Both bivariate and multivariate logistic regression analyses were performed to determine the association of obesity and other clinical parameters with mortality (defined as in-hospital death or transition to hospice care) and intensive care use (defined by transfer to intensive care unit [ICU]). Multivariate model was adjusted for demographics and 8 pertinent comorbidities.
Patients with obesity had higher risk of ICU admission (26.5% vs. 22.5%) and longer ICU stays (9.5±10.6 vs. 6.6±8.5 [days]; p<.05 for all) vs normal weight patients but mortality among the obese was lower (13.0% vs. 23.1%)
Obesity also was associated with a higher risk for both invasive (17.8% vs. 9.3%) and noninvasive (22.7% vs. 14.0%) ventilatory support.
Multivariate analysis found older age, male sex, and diabetes significantly associated with both mortality and ICU admission.
Individuals with severe obesity (BMI ≥ 40) were twice as likely to require ICU admission vs those with normal BMI (OR 2.07; 95% CI 1.51-2.82 for class III obesity).
“Our work underscores the impact of obesity on the course of COVID-19 and emphasizes the need to ensure that obesity is given appropriate consideration for risk stratification, vaccination protocols and in-hospital COVID-19 management,” emphasized Kang in the Endocrine Society release.
For more coverage of ENDO 2021, please click here.
