- Clinical Technology
- Adult Immunization
- Hepatology
- Pediatric Immunization
- Screening
- Psychiatry
- Allergy
- Women's Health
- Cardiology
- Pediatrics
- Dermatology
- Endocrinology
- Pain Management
- Gastroenterology
- Infectious Disease
- Obesity Medicine
- Rheumatology
- Nephrology
- Neurology
- Pulmonology
A Non-smoker with Progressive Dyspnea, No Cough
Dorothy is 55-years-old, has never smoked, and was well until 1 year ago when she first noticed mild dyspnea on exertion; it has gotten progressively worse.
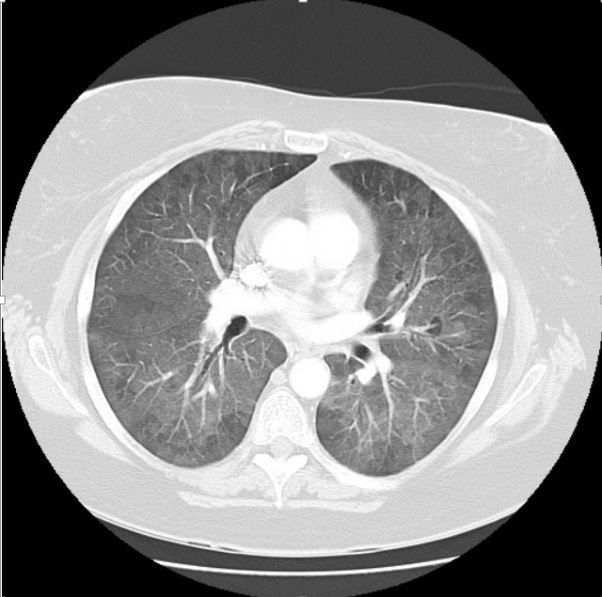
Figure. CT scan chest
Dorothy is a 55-year-old woman, who was well until about a year ago, when she first noticed some dyspnea carrying groceries up the front steps. This has progressed to where she now notes dyspnea even walking on level ground with her friends or at work. She recently had a hernia repair, and the preoperative chest xray showed increased interstitial markings. She was told to follow up with her physician, which is why she came into see you today. She denies cough and is a lifelong nonsmoker. She has no chest pain or any history of heart disease. She works as an accountant in Manhattan. She states that her office is old and dusty but knows of no mold problems at work or at home. She has no pets. She notes some back and neck arthritis but has no history of joint swelling, dry eyes or mouth, skin rashes, muscle pain, or change in color of digits in cold. Her only medications are an ACE inhibitor for hypertension, and occasional ibuprofen.
1. What possibilities are you considering for her shortness of breath and her radiographic findings?A. Idiopathic pulmonary fibrosis (IPF)
B. Interstitial lung disease (ILD) associated with connective tissue disease
C. Hypersensitivity pneumonitis
D. ILD associated with medications
E. ILD associated with occupational exposure (pneumoconiosis)
Please click below for answer, discussion, and continuation of case .
Answer: Actually, all of those conditions are reasonable possibilities. In fact, I would say that if you kept those 5 categories in mind, you would rarely miss a diagnosis in your approach to the patient with ILD. In this case, Dorothy is on the youngish side for IPF, but it is not unheard of for this to develop in a patient in his or her 50s. Most of my patients receive a diagnosis between the ages of 60 and 80, so when I see a patient below this age range, my radar for the other entities goes up. Dorothy denies any occupational exposure and is not taking any medications associated with ILD, so I would be concerned that she might have an undiagnosed connective tissue disease or hypersensitivity pneumonitis.
Physical Exam:
BP: 108/85 mm Hg; P: 68 beats/min; RR: 16 breaths/min; O2 sat: 98%; Wt: 125 lb; Ht: 5 ft 6 in
Skin: No rash
HEENT: No adenopathy
Lungs: Bibasilar crackles, positive inspiratory squeak
Heart: S1; S2; no murmurs, rubs, gallops
Abdomen: No organomegaly or tenderness
Extremities: No cyanosis, clubbing, or edema. No arthritic deformities, joint swelling or tenderness
2. Did the physical exam provide any further clues?
Definitely! The bibasilar crackles are consistent with the diagnosis of ILD. The inspiratory squeaks suggest a small airways problem, which really should point you to a specific category of disease, but I don’t want to give things away yet!
You obtain spirometry, screening bloodwork for collagen vascular disease, and a hypersensitivity pneumonitis panel; the results are shown in the Table below. You also walk the patient around your office, and she desaturates from 98% to 91%.
This is consistent with moderate restrictive disease, although you make a mental note to send the patient to a pulmonologist for full pulmonary function tests (PFTs), including lung volumes and diffusing capacity, to confirm.
Serologies for collagen vascular disease are negative. A hypersensitivity pneumonitis panel comes back positive for pigeon serum precipitating antibodies.
You then send the patient for a CT scan of the chest. A representative image is shown at right, above (please click image to enlarge).
Note the diffuse increased ground glass opacities throughout both lung fields. In addition, there are areas of relative sparing bilaterally as well, representing air trapping in the small airways. If expiratory films were obtained, these areas would become more pronounced, confirming this finding.
3. Now what is your diagnosis?
A. IPF
B. Hypersensitivity pneumonitis
C. ILD associated with collagen vascular disease
D. ILD associated with medications
E. ILD associated with occupational exposure (pneumoconiosis)
Please click below for answer and discussion.
Answer: B. Hypersensitivity pneumonitis. It turns out that Dorothy had found some abandoned, injured baby pigeons in her yard, and had brought them into her basement for rehabilitation, where they have been staying over the past year. When asked why she didn’t tell you this in the first place, Dorothy said she didn’t consider them pets, and she also didn’t want to admit that she had them, because in retrospect, she recognized that when she went into the basement to tend to the birds, her symptoms would acutely worsen. (This is a history that I have seen repeatedly in my practice. Patients will routinely deny that they have pets, and specifically have to be asked about birds in the house, in the garage, etc.)
Dorothy was able to give her pigeons to a local wildlife center. She was referred to a local pulmonologist, who treated her with steroids for 3 months, and her symptoms rapidly improved.
Conclusion
Hypersensitivity pneumonitis is a relatively common form of ILD, which usually presents with progressive dyspnea, exposure to mold or other antigen, restriction on PFTs, and a CT scan with characteristic early findings of air trapping and centrilobular ground glass opacities. Left untreated, it can progress to end-stage lung disease, so it is important to recognize this entity early, where removal of the offending antigen and, if necessary, treatment with steroids can markedly improve outcome.
