- Clinical Technology
- Adult Immunization
- Hepatology
- Pediatric Immunization
- Screening
- Psychiatry
- Allergy
- Women's Health
- Cardiology
- Pediatrics
- Dermatology
- Endocrinology
- Pain Management
- Gastroenterology
- Infectious Disease
- Obesity Medicine
- Rheumatology
- Nephrology
- Neurology
- Pulmonology
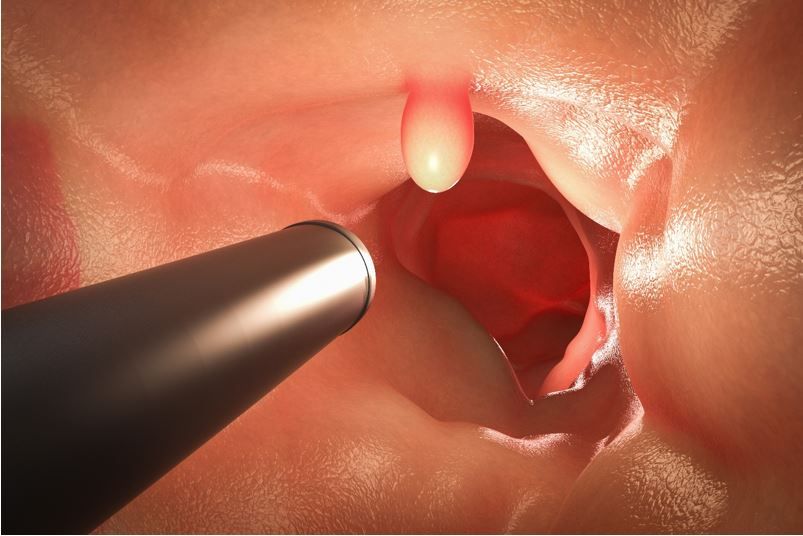
New Follow-Up Measure After Stool-Based CRC Test Could Improve Colonoscopy Rates, Outcomes
The quality performance measure is viable and reliable and could help improve early CRC detection rates via timely colonoscopy following abnormal stool-based test.
A novel quality performance measure that tracks rates of follow-up colonoscopy within 6 months of an abnormal stool-based screening test (SBT) for colorectal cancer (CRC) was found feasible and valid and had a median reliability of 94.5% across 38 health care organizations (HCO), according to a study published recently in JAMA Network Open.1
In the study, which included more than 20 000 adults between ages 50 and 75 years, 48% of participants received a colonoscopy within 6 moths after an abnormal SBT (fecal occult blood test, fecal immunochemical test, or multitarget stool DNA).
©phonlamaiphoto/shutterstock.com
“Stool-based tests are robust tools for CRC screening; however, their use only reflects part of the screening process. A timely follow-up colonoscopy following an abnormal SBT result is necessary to complete the screening process,” first author Elizabeth L Ciemins, PhD, MPH, MA, senior vice president of research and analytics at the American Medical Group Association, and colleagues wrote.1 Ideally, they added, this would happen “as soon as possible, but definitely within the 6 months after an abnormal test result. In fact, immediate follow-up should be emphasized due to the variation in stage at first cancer detection.”1
Impetus for development and testing of the new quality performance measure reflects sobering findings on outcomes including research that found individuals with a positive SBT who did not pursue a follow-up colonoscopy were twice as likely to die as those who did follow-up with the test.2 According to the authors, the measure would complement and augment the value of the existing Healthcare Effectiveness Data and Information Set measure, which captures only the first step in the screening process.1
For the retrospective quality improvement study, Ciemins and colleagues tapped deidentified electronic health record data from the Optum Labs Data Warehouse for the period from January 2016 to December 2020. The primary outcome measure specified for the study was the proportion of adults aged 50 through 75 years with a completed colonoscopy within 180 days following an abnormal SBT result, with 2018 identified as the primary measurement year, according to the study. Reliability of the measure was calculated across HCOs, participant race, ethnicity, and measurement year. Follow-up rates were recorded by race, ethnicity, sex, insurance, and type of test.
FINDINGS1
The final study population comprised 20 581 adults (mean age, 63.6 years; 51.4% women; 86% White) across 38 HCOs who had an abnormal SBT result for CRC during 2018.
The researchers reported a median of 47.9% of participants underwent a follow-up colonoscopy within 6 months, with a median follow-up of 53 days. Researchers noted “significant variation” between HCOs, finding a range in performance from 13.1% to 69.9%. Follow-up rates also differed across years and increased by approximately 33% between 2016 and 2019, a change study authors said indicates “the ability of HCOs to improve performance rates.” Follow-up rates then declined by 14% through 2020, likely an artifact of the COVID-19 pandemic.
Documented disparities in CRC screening rates were also observed in this study. The highest follow-up rates in 2018 were among White participants (49%; 95% CI, 48.2-49.7) compared with Black (37.1%; 95% CI, 34.6-39.5) and Hispanic participants (38.4%; 95% CI, 34.6-42.1). Rates also differed by type of insurance and were highest for those with commercial insurance (50.9%; 95% CI, 50-51.7) compared with Medicare (49.2%; 95% CI, 47.7-50.6) or Medicaid (39.2%; 95% CI, 36.6-42.1), all P <.001.
Analysis of the performance measure’s reliability found a median of 94.5% variance derived from differences between HCOs (range, 74.3%-99.7%). Reliability rates for other categories were also high, at 94.2% (79.5%-99.5%) for race, 93.1% (86.7%-99.4%) for ethnicity, and 99.3% (99.1%-99.4%) for year of measurement year, according to the findings.
Feasibility testing of the measure found that “most data elements were feasible to capture in the [electronic health record]. Hospital stay and emergency department visit were not uniformly available but participating organizations did indicate the capacity to differentiate between screening and diagnostic SBT, wrote authors.
“The measure was reliable, with variation between systems due to differences in performance, and was a feasible means of calculation and reporting using EHR data,” said the team. “Ultimately, we hope to improve CRC screening rates and detection of CRC at earlier stages in efforts to reduce the burden of this disease on individuals and health care systems,” they concluded.
