
- Clinical Technology
- Adult Immunization
- Hepatology
- Pediatric Immunization
- Screening
- Psychiatry
- Allergy
- Women's Health
- Cardiology
- Pediatrics
- Dermatology
- Endocrinology
- Pain Management
- Gastroenterology
- Infectious Disease
- Obesity Medicine
- Rheumatology
- Nephrology
- Neurology
- Pulmonology
New Antivirals for Hepatitis C: Four Basic Facts
A new era in hepatitis C treatment began in May 2011, with approval of telaprevir and boceprevir. They are effective only for some patients, but new and better options are well on their way to the clinic.
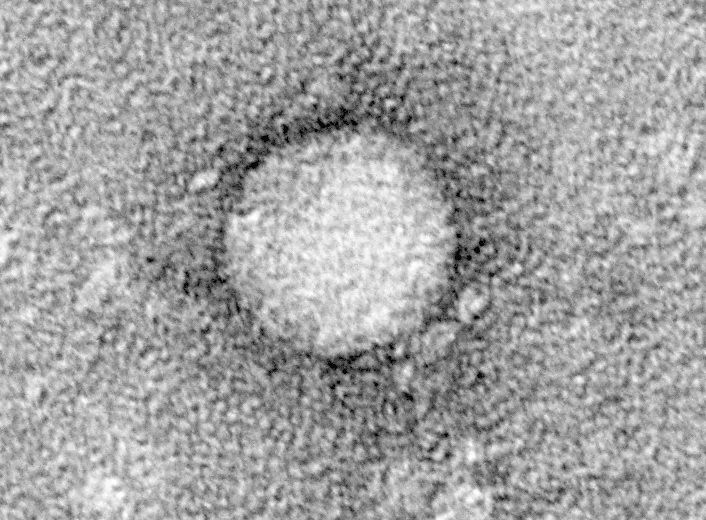
A new era in the treatment of hepatitis C virus (HCV) began in May 2011, with the approval of Incivek (telaprevir) and Victrelis (boceprevir), the first two commercially available agents in a new class of direct-acting antiviral agents (DAAs) that are specifically designed to inhibit HCV proteins. Although they improve on current treatment options, even better versions are anticipated within the near future that should substantially increase the proportion of HCV patients who can receive effective therapy.
These new agents are described in detail in a recent review.1 Here, I highlight the most important implications for those who treat the rheumatic disorders resulting from hepatitis C infection.
1. The burden of liver disease caused by hepatitis C virus (HCV) is increasing in the United States, where approximately 4 million persons are estimated to be chronically infected.2,3 Beyond being a major cause of rheumatic disorders, infection with HCV can lead to progressive liver fibrosis and cirrhosis that in turn can cause end-stage liver disease and/or hepatocellular carcinoma, which are fatal in the absence of liver transplantation. The goal of HCV therapy is to prevent these serious complications of chronic infection by eradicating the virus permanently with a finite course of treatment.
2. Response rates to traditional therapy with pegylated intereferon alfa (Peg-IFN) and ribavirin (RBV) were suboptimal. In patients with genotype 1 HCV (the most common viral strain in the US and the most difficult to treat), only 40-50% of patients experience sustained viral clearance following 48 weeks of therapy with Peg-IFN and RBV.4 The response rate is even lower in certain patient populations, including:5-7
• those who have failed to benefit from a prior course of therapy,
• those with advanced hepatic fibrosis or cirrhosis,
• those who are resistant to insulin, and
• African American patients.
In addition, interferon-based HCV therapy has been poorly tolerated or contraindicated in a large subset of patients, including those with autoimmune disorders, decompensated liver disease, cytopenias, or psychiatric disorders.8 Furthermore, the mechanism of antiviral activity in these drugs is poorly understood.
3. Adding either telaprevir or boceprivir to Peg-IFN and RBV markedly increases response rates in the most prevalent group of HCV-infected patients, but many are still unable to benefit.The combinations are significantly more effective among genotype 1 patients who are nave to or have failed a prior course of therapy.9-12 However, because both agents require concomitant use of Peg-IFN and RBV, patients intolerant of IFN or in whom it is contraindicated (including those with autoimmune disorders) are unable to receive the currently available protease inhibitor-based triple therapy.
Also, there are some noteworthy adverse effects. Significant anemia is common with both agents, and telaprevir use has been associated with a rash that can be serious in some individuals.
4. The development of new DAAs with greater potency and more favorable side effect profiles is evolving rapidly, with increasing evidence that most if not all patients with HCV will eventually be able to be cured with shorter courses of DAAs +/- Peg-IFN or RBV or, most excitingly, with IFN-free combinations of oral anti-HCV agents. The two newly available agents are NS3/4A protease inhibitors.Newer NS3/4A protease inhibitors are in development, as well as agents that inhibit NS5B polymerase and others that inhibit the multifunctional NS5A protein.
It appears that patients with the more favorable genotype 2 and 3 HCV likely will be treated with a highly potent DAA in combination with RBV. Patients with genotype 1 HCV likely will receive either more DAAs alone, in combination with RBV, or (for those most difficult to treat because of prior treatment failures) combined with both Peg-IFN and RBV.
The first of these next-generation DAAs are anticipated to be available for prescribing within the year. Several more will likely follow them into the marketplace in the next 2-3 years. The challenge facing practitioners at present is the difficult decision of weighing the urgency to treat patients with currently available protease inhibitor-based triple therapy against the risks of waiting for the more potent, better tolerated novel agents.
References:
REFERENCES
1. Jesudian AB, de Jong YP, Jacobson IM. Emerging therapeutic targets for hepatitis C virus infection.Clin Gastroenterol Hepatol (2013) 11(6):612-619.
2. Davis GL, Alter MJ, El-Serag H et al.Aging of hepatitis C virus (HCV)-infected persons in the United States: a multiple cohort model of HCV prevalence and disease progression.Gastroenterology (2010) 138:513521.
3. Armstrong GL, Wasley A, Simard EP et al.The prevalence of hepatitis C virus infection in the United States, 1999 through 2002. Ann Intern Med (2006) 144:705-714.
4. McHutchison JG, Lawitz EJ, Shiffman ML et al.Peginterferon alfa-2b or alfa-2a with ribavirin for the treatment of hepatitis C infection.N Engl J Med (2009) 361:580-593.
5. Conjeevaram HS, Fried MW, Jeffers LJ et al.Peginterferon and ribavirin treatment in African American and Caucasian American patients with hepatitis C genotype 1.Gastroenterology (2006) 131:470–477.
6. Reddy KR, Shiffman ML, Rodriguez-Torres M, et al.Induction pegylated interferon alfa-2a and high dose ribavirin do not increase SVR in heavy patients with HCV genotype 1 and high viral loads.Gastroenterology (2010) 139:1972–1983.
7. Romero-Gómez M, Del Mar Viloria M, Andrade RJ et al.Insulin resistance impairs sustained response rate to peginterferon plus ribavirin in chronic hepatitis C patients.Gastroenterology (2005) 128:636–641.
8. World Health Organization. Global Alert and Response (GAR): Hepatitis C. (2002) Accessed June 4, 2013
9. Jacobson IM, McHutchison JG, Dusheiko G et al.Telaprevir for previously untreated chronic hepatitis C virus infection.N Engl J Med (2011) 364:2405–2416.
10. Zeuzem S , Andreone P , Pol S, et al.Telaprevir for retreatment of HCV infection.N Engl J Med (2011) 364:2417–2428
11. Poordad F, McCone J, Bacon BR et al.Boceprevir for untreated chronic HCV genotype 1 infection.N Engl J Med 2011;364:1195–1206.
12. Bacon BR, Gordon SC, Lawitz E et al.Boceprevir for previously treated chronic HCV genotype 1 infection.N Engl J Med (2011) 364:1207–1217.
FDA Approves Guselkumab for Pediatric Plaque Psoriasis and Active Psoriatic Arthritis
September 30th 2025The FDA has approved guselkumab for children aged 6 years and older with moderate to severe plaque psoriasis or active psoriatic arthritis, making it the first IL-23 inhibitor authorized for pediatric use.
FDA Approves Guselkumab for Pediatric Plaque Psoriasis and Active Psoriatic Arthritis
September 30th 2025The FDA has approved guselkumab for children aged 6 years and older with moderate to severe plaque psoriasis or active psoriatic arthritis, making it the first IL-23 inhibitor authorized for pediatric use.
2 Commerce Drive
Cranbury, NJ 08512
All rights reserved.