- Clinical Technology
- Adult Immunization
- Hepatology
- Pediatric Immunization
- Screening
- Psychiatry
- Allergy
- Women's Health
- Cardiology
- Pediatrics
- Dermatology
- Endocrinology
- Pain Management
- Gastroenterology
- Infectious Disease
- Obesity Medicine
- Rheumatology
- Nephrology
- Neurology
- Pulmonology
Neurological Nemeses: A Photo Essay
Neurofibromatosis, neuroretinitis, neurologic complications of Down syndrome, Lhermitte-Duclos disease, neurosarcoidosis-find insights here for defeating nervous system disorders.

Case 1:
Multiple randomly distributed, flesh-colored nodules were noted on the trunk, arms, and face of a 62-year-old man. The lesions measured 0.5 to 1.0 cm and appeared slightly pedunculated. He had had the lesions since he was a teenager; they were not painful. Tissue biopsy confirmed the suspected diagnosis of neurofibromatosis type I.
Neurofibromatosis may occur sporadically or follow a familial distribution. Type I manifests as flesh-colored nodules (neurofibromas) randomly distributed throughout the body. Type II manifests as axillary freckling and skin pigmentation disruptions (caf au lait spots). It is associated with eighth cranial nerve tumors of multiple endocrine neoplasia.
Systemic complications that have been associated with neurofibromatosis include meningiomas, gliomas, mental retardation, obstructive hydrocephalus, and peripheral sarcomas.
NEXT CASE »
For the discussion, click here.

Case 2:
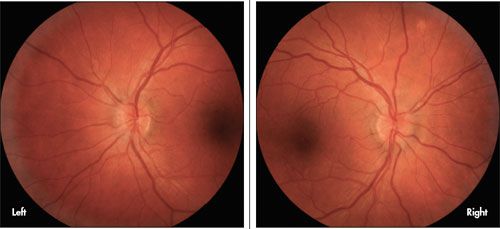
A 17-year-old sexually active woman presented with sudden vision loss in her left eye. She recently had a viral illness. The only change in her home environment was a new kitten. The fundus examination is shown. There was a relative afferent pupillary defect in her left eye. The diagnosis was cat scratch disease–related neuroretinitis.
Cat scratch disease (CSD)-related neuroretinitis is caused by Bartonella henselae, a pleomorphic gram-negative intracellular bacillus. About 22,000 cases of CSD are reported in the United States each year, but neuroretinitis affects only 1% to 2% of infected patients.
Serologic testing is helpful for diagnosis, prognosis, and to guide treatment with antibiotics. Initial investigations should include a general physical examination; an inoculation papule can be found in up to 90% of infected patients. Complete blood cell count and blood and serological studies for other causes of neuroretinitis (eg, syphilis, Lyme) could also be performed.
Case and image courtesy of Jahangir Kabir, MD, Adeel Khan, MD, and Andrew G. Lee, MD
NEXT CASE »
For the discussion, click here.
Case 3:
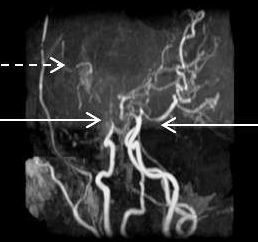
Children with Down syndrome are at risk for medical complications that may affect the neurologic and other systems. Moyamoya syndrome is a cerebrovascular disorder characterized by progressive noninflammatory, nonatherosclerotic occlusion of bilateral intracranial arteries with compensatory formation of fragile arterial collateral vessels (below) that maintain cerebral circulation. This classic complication leads to stroke.
Neurologic issues that may arise while providing medical care to children with DS include hypotonia,epilepsy, impaired intellectual development, psychiatric problems, cervical cord compression, and vision and hearing impairment.
Article and image provided by Lalitha Sivaswamy, MD
NEXT CASE »
For the discussion, click here.
Case 4:
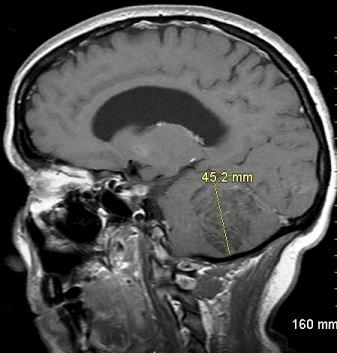
A 39-year-old woman presented with a 2-month history of progressively worsening headache and right-sided ataxia. Neurologic examination revealed mild dysmetria, and dysdiadochokinesia on the right side. MRI of the brain demonstrated a 4.5-cm, nonenhancing, T1 hypointense mass on the right cerebellar hemisphere. This MRI finding is consistent with Lhermitte-Duclos disease.
LDD, or dysplastic gangliocytoma of the cerebellum, is a rare, slow-growing, benign lesion of the cerebellum. It is often asymptomatic in early life but usually becomes clinically apparent in the third and fourth decades.
The clinical manifestations of LDD are usually related to a posterior fossa mass-effect and the secondary obstructive hydrocephalus that follows. The most frequent complaints are headaches and ataxia (70% of patients). Cerebellar signs and symptoms are seen in 40% to 50% of patients and may be present for years before diagnosis. One-third of patients have associated cranial nerve palsies and long tract dysfunction. Less commonly noted presenting features are visual problems, neck stiffness, vertigo, and subarachnoid hemorrhage.
Case and image courtesy of Wikrom Warunyuwong, MD, Wisit Cheungpasitporn, MD, Daych Chongnarungsin, MD, Yasemin S. Tashman, MD, and Sirisak Chanprasert, MD
NEXT CASE »
For the discussion, click here.
Case 5:
A 36-year-old man had a dark spot in the field of vision of his left eye that now more closely resembled a line. An earlier workup was unremarkable except for an elevated C-reactive protein level and a mild prominence of the left hilum on his chest radiograph. Examination of the optic discs through dilated pupils revealed bilateral papilledema, more prominent at the nasal disc margins. Non-necrotizing granulomas seen in a transbronchial biopsy would demonstrate neurosarcoidosis.
Optic nerve dysfunction is the most common neuro-ophthalmological manifestation of sarcoidosis, and the optic nerve is said to be the second most commonly affected cranial nerve after the facial nerve.
The optic nerve may be affected at any time during the course of the disease and may be the site of its initial presentation. Papilledema, as seen in this patient, may result from the elevated intracranial pressure, which is often associated with neurosarcoidosis.
Case and images provided by Leonid Skorin, Jr, DO
