- Clinical Technology
- Adult Immunization
- Hepatology
- Pediatric Immunization
- Screening
- Psychiatry
- Allergy
- Women's Health
- Cardiology
- Pediatrics
- Dermatology
- Endocrinology
- Pain Management
- Gastroenterology
- Infectious Disease
- Obesity Medicine
- Rheumatology
- Nephrology
- Neurology
- Pulmonology
The Neurohormonal Axis of the Left Atrial Appendage
A small single-center study yields provocative results that may help increase understanding of the importance of the left atrial appendage.
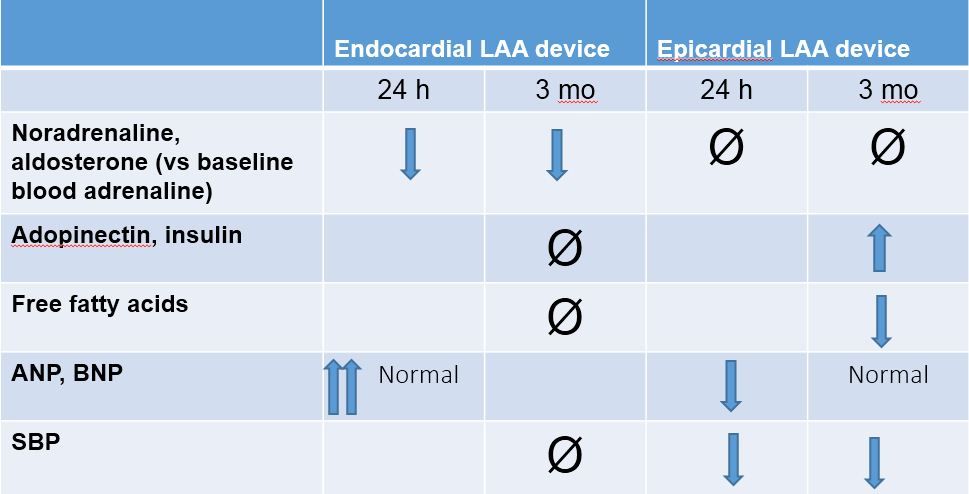
Table. (Please click to enlarge)
The purpose of the left atrial appendage (LAA) continues to confuse cardiologists worldwide. Initially, it was thought to be a fetal remnant but more recently, we are learning that the LAA may have mechanical and hormonal actions as well. A recent analysis (reviewed onPatient Care) looking at LAA exclusion during cardiac surgery not related to atrial fibrillation (AF) revealed a higher short-term incidence of post-operative AF (reference other article) without a change in ischemic stroke and mortality outcomes.
The LAA HOMEOSTASIS study, a small, single-center study published recently in JACC, looked at the impact of LAA exclusion on systemic homeostasis. The study compared 38 patients undergoing Lariat suture ligation (epicardial closure) with 39 patients undergoing Watchman (endocardial closure) procedures. Neurohormones that originate from the left atrium and LAA (ANP and less so, BNP) as well as adrenergic hormones (epinephrine, norepinephrine), the renin-angiotensin and aldosterone system hormones, and the metabolism hormones (adiponectin, free fatty acids, insulin, β-hydroxy butyrate, free glycerols) were measured immediately before the procedure, immediately after device deployment, at 24 hours, and at 3 months follow-up. The hormonal profile in the aftermath of the two types of closures were dramatically different with significant differences in measured hormones, systemic blood pressure profiles, and physiologic responses (see Table; please click to enlarge).
This study sheds light not only on the hormonal role of the LAA but also on how different occlusion techniques can alter systemic physiologic and endocrinologic responses. After studies such as this one, we realize that as we progress in the world of AF management with advances such LAA occlusion becoming more widespread, we need to better understand the full range of consequences associated with them.
Source: Lakkireddy D, Turagam, Afzal MR, et al. Left atrial appendage closure and systemic homeostasis: the LAA HOMEOSTASIS study. JACC. 2018;71:135-144; DOI:10.1016/j.jacc.2017.10.092
