- Clinical Technology
- Adult Immunization
- Hepatology
- Pediatric Immunization
- Screening
- Psychiatry
- Allergy
- Women's Health
- Cardiology
- Pediatrics
- Dermatology
- Endocrinology
- Pain Management
- Gastroenterology
- Infectious Disease
- Obesity Medicine
- Rheumatology
- Nephrology
- Neurology
- Pulmonology
Mild Asthma, Poorly Controlled: A Case In Point
"Cindy" says she's using her albuterol inhaler up to 6 times a day, but her asthma is worse. A pulmonologist poses 4 questions that can lead to preferred Rx.
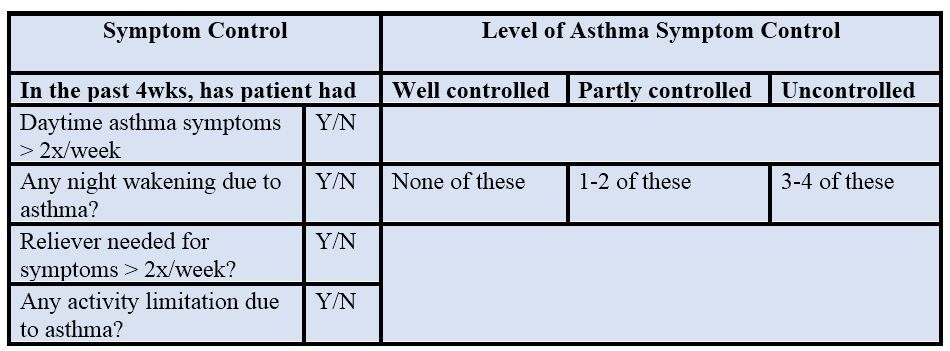
Table 2 (Please click to enlarge)
Cindy is a 23-year-old female, with a history of asthma that was diagnosed when she was age 8. Over the past month, she has noticed that her asthma is getting worse. She notes that she can’t play soccer anymore without having to stop and take her rescue inhaler, and that she has had 3 asthma attacks that have awakened her. Cindy uses albuterol by metered dose inhaler for rescue medication, and mometasone inhaler (Asmanex Twisthaler 220 mcg) once daily as a controller. She states that she has been using her albuterol inhaler daily, sometimes as much as 6 times a day.
Question 1: What is the most likely reason for Cindy’s worsening asthma symptoms?1. She doesn’t have asthma, but something else
2. She’s using her inhaler incorrectly
3. New environmental problem
4. She’s not compliant with her controller medications
5. Cindy’s asthma has worsened, and she now needs additional controller medication
6. Cindy has developed worsening allergies and reflux, which in turn have contributed to her worsening asthma
Please click below for answer and discussion.
Answer: These are all good answers, and actually represent a checklist that I go through when I see a patient with worsening asthma.
However, if I had to pick the most likely answer for Cindy, I would pick answer 4, (compliance with controller medication), followed closely by answer 2, (incorrect use of inhaler).
Patients’ with asthma are notoriously poorly compliant with controller medication. Furthermore, even when they do remember to take their inhaler, they often do so incorrectly (answer 2). Only a small minority of patients actually use their controller medication correctly and on time.1 I always make it a point to ask patients to demonstrate their technique with their inhaler in the office directly to me. This serves 2 purposes:
First, it shows the patient that you, the treating physician, think that their controller medication is important enough that you are willing to take time out of your busy day to watch them perform the maneuver.
Second, you can critique their technique, and determine if they are getting the medication that you prescribed into their lungs. If they aren’t, it’s time to try a different type of device.
Let’s move along to the physical exam and spirometry:
Physical Exam:
BP: 108/85 mm Hg, P: 68, RR: 16, O2 sat: 98%, Wt: 125 lbs, Ht: 5’ 6”
Skin: No rash
HEENT: No adenopathy
Lungs: positive expiratory wheezing
Ht: S1, S2, no murmurs rubs gallops
Abd: No organomegaly or tenderness
Extremities: No cyanosis, clubbing, or edema. No arthritic deformities, joint swelling or tenderness
Table 1. Spirometry results
These results are consistent with moderate obstructive disease with a bronchodilator response, consistent with asthma.
Question 2: What diagnoses should we consider other than asthma?
1. Vocal cord dysfunction
2. COPD
3. CHF
4. Medication-related cough
5. Small airways disease
6. Pulmonary embolism
7. Central airway obstruction
Please click below for answer and discussion.
Answer: These are all reasonable alternatives to asthma in adults.
Cindy, with documented intermittent wheezing, marked reversibility of obstruction on spirometry, and no history to suggest an alternative diagnosis, certainly has asthma. In general, however, asthma may be greatly over-diagnosed in the general population. A recent study suggested that about 1 of 3 patients diagnosed with asthma does not have the disease.2
One of the more common entities that needs further mention is vocal cord dysfunction. Usually, patients with this disorder will have abnormal adduction of their vocal cords during inspiration, causing stridor, but expiratory adduction can occur as well. It is also episodic, and-to make life more complicated-can often coexist with asthma. I often consider this diagnosis in patients who have poor control of asthma despite maximal therapy, those with predominantly inspiratory wheezing, those with evidence of stridor on physical exam or spirometry, and those with dysphonia or other throat symptoms in between attacks. Referral to an ENT specialist with a special interest in this disease is crucial.
Question 3: How would you characterize Cindy’s asthma?1. Mild asthma with poor control
2. Moderate asthma with good control
3. Moderate asthma with poor control
4. Severe asthma with poor control
Please click below for answer and discussion.
Answer: The answer, according to the current GINA (Global Initiative for Asthma) guidelines,3 is mild asthma with poor control.
Let’s discuss asthma control first. Asthma symptom control refers to the patient’s current state on his or her present therapy. There are a number of questionnaires and guidelines that can help determine the level of control. The recommended one from the GINA guidelines is summarized in Table 2 above (please click to enlarge).
Cindy has experienced all 4 of these symptoms, so her asthma is classified as uncontrolled.
Severity is determined retrospectively, by the amount of medicine used to control the patients’ asthma over the past several months. Patients can be classified into 5 steps and recommended preferred treatments as shown in Table 3, below, also as recommended by GINA.
Table 3. Stepwise approach to controlling asthma symptoms
ICS, inhaled corticosteroid; LABA, long-acting bronchodilator; LAMA, long-acting muscarinic antagonist
Cindy, at least until recently, had been controlled on step 2. Steps 1 and 2 are considered mild asthma, step 3 is moderate asthma, and steps 4 and 5 are severe asthma. Thus, at least for now, Cindy has mild asthma. However, if she eventually requires control at a higher level for months, then her severity level will change accordingly.
Question 4: Let’s assume Cindy has good technique and adherence to therapy, has no modifiable risk factors such as a new pet or smoking, and no comorbidities, and we have ruled out other entities such as vocal cord dysfunction. How would you change therapy?1. Add a long-acting beta agonist (LABA) to the current regimen of Asmanex
2. Change to a combination low dose ICS/LABA
3. Change to a medium dose ICS
4. Add a leukotriene receptor antagonist, such as montelukast
5. Add theophylline
Please click below for answer and discussion.
Answer: The preferred treatment is a combination low dose ICS/LABA.
Although answers one and two seem identical, they are not. Adding a separate LABA to an ICS in asthma is dangerous. Many patients will not adhere to the multiple inhaler regimen, and will take the LABA by itself. This can lead to the ‘masking’ of inflammation, and studies have clearly shown worse asthma outcomes and even excess asthma deaths with this regimen. The other alternatives, 3-5, are all reasonable, and might even be a better choice for an individual patient, but the preferred choice is choice 2.
Conclusion
Cindy has had mild asthma, but it is now poorly controlled. This case report highlights my approach to a patient such as Cindy, and I hope it helps you in your daily office practice.
References
1. Bonds RS, Asawa A, Ghazi A. Misuse of medical devices: a persistent problem in self-management of asthma and allergic disease. Ann Allergy Asthma Immunol 2015;114:74-75.
2. Aaron SD, Vandemheen KL, FitzGerald JM, et al. Reevaluation of diagnosis in adults with physician-diagnosed asthma. JAMA.
2017;317:269-279.
3.Global Initiative for Asthma. Accessed February 2, 2018.
Kymera's Oral STAT6 Degrader KT-621 Shows Biologic-Like Activity in Early Atopic Dermatitis Trial
December 8th 2025KT-621 achieved deep STAT6 degradation and strong 4-week EASI and itch reductions, offering a potential new oral option for moderate–severe AD and other Th2 inflammation-driven disease.
