- Clinical Technology
- Adult Immunization
- Hepatology
- Pediatric Immunization
- Screening
- Psychiatry
- Allergy
- Women's Health
- Cardiology
- Pediatrics
- Dermatology
- Endocrinology
- Pain Management
- Gastroenterology
- Infectious Disease
- Obesity Medicine
- Rheumatology
- Nephrology
- Neurology
- Pulmonology
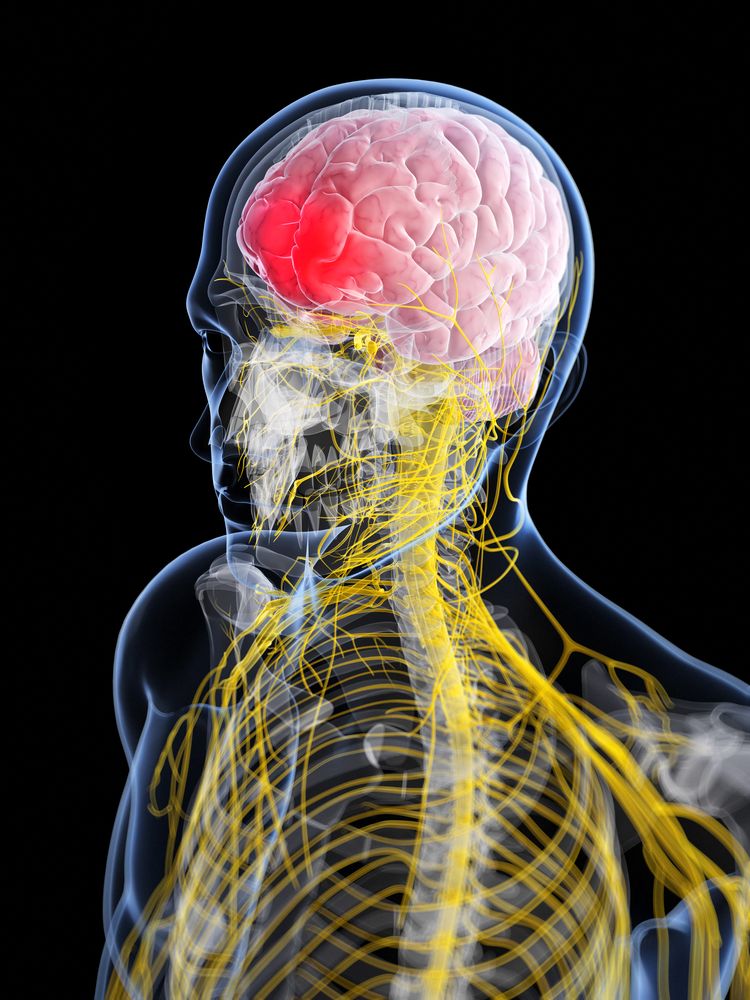
Migraines, Cardiovascular Risk, & Vasoconstrictors
Migraine-especially with aura-is a CV risk factor, which makes treatment with ergots or triptans potentially problematic. The best approach?
©Sebastian Kaulitzki / Shutterstock.com
About 900,000 Americans who have episodic migraine may be at high cardiovascular risk. This makes use of commonly prescribed migraine medications potentially problematic.1
CV comorbidities are common in migraine sufferers, for whom the risk for CV events and mortality is increased. Ergots and triptans can cause vasoconstriction and are contraindicated in patients with CV comorbidities. The FDA therefore advises caution when using vasoconstrictors in such patients, and recommends a CV evaluation for patients with CV risk factors who have not previously used these drugs.
A previous study by the authors of the newly published American Migraine Prevalence and Prevention (AMPP) Study found that 2.6 million Americans with episodic migraine are at high CV risk.2 But that study only looked at people who had already had CV procedures. It did not include migraine sufferers at risk for a first CV event, who may fly under the radar when prescribed a migraine medication.
To gain a fuller perspective, researchers used data from the 2009 AMPP study. Questionnaires were mailed to 120,000 households representative of the US population. Of these, researchers selected a random subset with severe headache for longitudinal follow-up using questionnaires mailed annually.
The analysis included 6723 people from the longitudinal subset who were aged ≥22 years and had episodic migraine. The population included 5227 women, 1496 men, and was about 90% white. Researchers assessed CV risk using past history of CV events/procedures and 10-year risk for CV events using the Framingham Risk Score (FRS). People with ≥30% increased FRS were considered to be at high CV risk. Researchers also extrapolated their findings to the US population using 2015 US census data.
KEY FINDINGS
. National Projection: 403,000 women and 510,000 men had episodic migraine with high FRS and/or past CV event or procedure
. Women: 40-59 years: 69,000; ≥60 years: 334,000
. Men: 40-49 years: 197,000; ≥ 60 years: 313,000
. People with episodic migraine at risk for a first CV event in the next 10 years:
. Women: 40-59 years: 0.4%; ≥60 years: 8.2%
. Men: 40-59 years 5.3%; ≥60 years: 31.7%
Although the percentage of those at risk for a first CV event in the next 10 years was about 4 times higher in men ≥ 60 years compared to women in the same age group, the prevalence of episodic migraine is 3 times higher in women vs men. So the projected number of women in this group is about the same as men (181,000 vs 187,000, respectively).
The authors stressed that migraine with aura represents one of the most important CV risk factors in women, second only to hypertension. The results underscore the importance of remaining vigilant to CV disease in women.
“CV disease is both underrecognized and undertreated in women. In fact, CV disease is the leading cause of premature death of women in the US and is responsible for one in three female deaths in the US,” wrote first author Richard Lipton, MD, of Albert Einstein College of Medicine and Montefiore Headache Center (Bronx, NY), and colleagues.
The authors also noted several implications for clinical practice:
- First, clinicians should assess cardiac history as well as CV risk factors in patients with migraine, and obtain a thorough CV history before prescribing vasoconstrictors.
- Patients who were free of CVD when initially prescribed these medications should receive periodic CV risk assessments over time.
- Finally, non-vasoconstrictive treatments may play an important role in the acute treatment of migraine, especially in women ≥ 60 years and men ≥ 40 years.
THE TAKE HOME POINTS
• About 900,000 Americans with episodic migraine are at high CV risk and/or have had a past CV event or procedure, making the prescription of ergots or triptans potentially problematic for these patients
• Over 360,000 women and men aged 60+ who have episodic migraine may be at risk for a first CV event in the next 10 years
• Clinicians should assess CV history and CV risk factors before prescribing ergots or triptans, and periodically assess CV risk factors in patients on these medications over time
• Women are at higher risk for episodic migraine than men, and clinicians should remain vigilant to CV disease in women
References:
1. Lipton RB, Reed ML, Kurth T, et al. Framingham-based cardiovascular risk estimates among people with episodic migraine in the US population: results from the American Migraine Prevalence and Prevention (AMPP) Study. Headache. 2017 Oct 9.
2. Buse DC, Reed ML, Fanning KM, et al. Cardiovascular events, conditions, and procedures among people with episodic migraine in the US population: results from the American Migraine Prevalence and Prevention (AMPP) Study. Headache. 2017;57:31-44.
