- Clinical Technology
- Adult Immunization
- Hepatology
- Pediatric Immunization
- Screening
- Psychiatry
- Allergy
- Women's Health
- Cardiology
- Pediatrics
- Dermatology
- Endocrinology
- Pain Management
- Gastroenterology
- Infectious Disease
- Obesity Medicine
- Rheumatology
- Nephrology
- Neurology
- Pulmonology
Isolated Acute Posterior Myocardial Infarction in a Middle-Aged Man
Figure 1. 12-lead ECG tracing. (Click each image to enlarge)
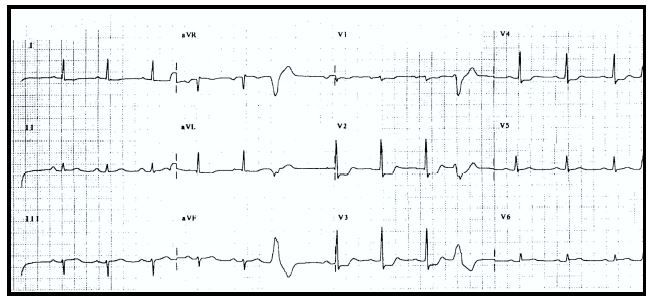
Figure 2. Isolated APMI. Note ST segment depression in leads V1 to V4.
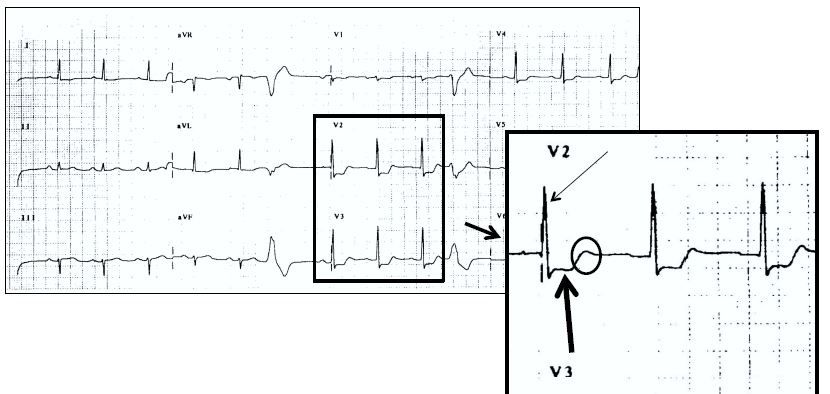
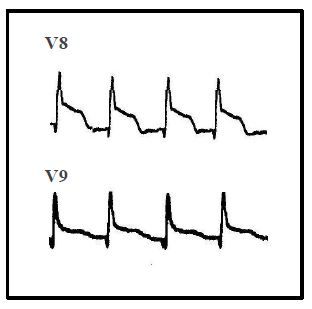
Figure 3. Posterior leads V8 and V9.
A 54-year-old man with history of hypertension and tobacco use presented to the emergency department with chest pain. The patient noted the onset of chest pain approximately 45 minutes before presentation; he described the sensation as an ache and said it was associated with nausea and diaphoresis. The patient’s medications included aspirin and metoprolol.
On examination, he was alert, oriented, anxious, and in moderate distress with significant diaphoresis. Vital signs were blood pressure, 118/88 mm Hg; pulse, approximately 80 beats/min; respiratory rate, 28 breaths/min; temperature, 37.1°C (98.8°F); and oxygen saturation, 94% on room air. The ECG monitor demonstrated the normal sinus rhythm with occasional premature ventricular contractions. The cardiac and pulmonary examinations were normal; the remainder of the examination was unrevealing. A 12-lead ECG was performed (Figure 1). Laboratory studies were obtained and a chest radiograph was ordered.
Based on the clinical presentation and the ECG in Figure 1, the most likely diagnosis is:
A. Acute posterior wall myocardial infarction.
B. Anterior wall ischemia.
C. The strain pattern of left ventricular hypertrophy (by voltage).
D. Left main acute coronary syndrome pattern.
Ansewr: A. Acute posterior wall myocardial infarction.
Discussion
Acute posterior wall myocardial infarction (APMI) represents 15% to 20% of all MIs. The coronary lesion responsible for APMI is most often found in the distal circumflex artery or a continuing branch of the right coronary artery, termed the posterior descending branch. Considering the coronary anatomy involved in this infarction, it is very understandable that APMI is most often associated with ST-segment elevation MI (STEMI) of either the inferior or lateral walls of the left ventricle; however, isolated APMI does occur, seen in approximately 5% to 7% of all acute myocardial infarctions (AMIs).
In leads V1 through V3, the posterior wall of the left ventricle is viewed indirectly from the perspective of the anterior wall. In patients suspected of having acute coronary syndrome (ACS), ST-segment depression in leads V1 through V4 is a result of either anterior wall ischemia or APMI. Using the standard 12-lead ECG (Figure 2), APMI often presents with horizontal, or flat, ST-segment depression in the anterior leads (leads V1 through V4); prominent R waves in leads V1 and/or V2; an R/S ratio greater than 1.0 in leads V1 and/or V2; and an upright T wave in leads V1 and/or V2. These additional ECG features increase the likelihood that APMI is responsible for the ST-segment depression.1
Additional ECG evidence of APMI is obtained by using posterior ECG leads V8 and V9(Figure 3). These additional leads (V8 and V9), placed on the posterior thorax, directly image the posterior wall of the left ventricle. ST-segment elevation of 1 mm or more can indicate APMI. Many experienced clinicians are comfortable diagnosing APMI with the 12-lead ECG; if needed, these additional ECG leads can be used as well.
Management of APMI is relatively straightforward should it occur in the setting of simultaneous inferior or lateral STEMI. In this situation, the clinician must initiate standard anti-ischemic therapies while also using antiplatelet and anticoagulant treatments, assuming no contraindication is present. These therapies are initiated while emergent reperfusion (fibrinolysis or percutaneous coronary intervention [PCI]) is prepared. The management of isolated APMI is somewhat controversial. One strategy suggests the use of an approach similar to that used for NSTEMI: anti-ischemic, antiplatelet, and anticoagulant therapies are started; the patient is then taken to the cardiac catheterization laboratory for non-urgent coronary angiography with or without PCI. Others note that the isolated APMI is an acute infarction of a wall of the left ventricle most frequently the result of from an occluded epicardial coronary artery, and thus the patient should undergo urgent PCI, similar to the management approach of STEMI. While volumes of data do not exist supporting this more aggressive approach, the concept of opening closed arteries as rapidly as possible, thus restoring perfusion to the damaged myocardium, is likely the better option.
Case Conclusion
The ECG in Figure 1 demonstrated significant ST-segment abnormalities in addition to other findings. The patient was quite ill-appearing with a presentation suggestive of AMI. The differential consideration included anterior wall ischemia (ie, non-infarction ACS) versus APMI. Point-of-care laboratory tests revealed normal troponin, serum chemistries, glucose, and hematocrit; the portable chest radiograph was normal. Antiplatelet and anticoagulant therapies were started; judicious use of sublingual nitroglycerin was made while a normal saline intravenous fluid bolus was performed. Cardiology was urgently consulted; on review of the ECG electronically from a distant site, the cardiologist recommended urgent PCI for a presumed APMI. At cardiac catheterization, a distal circumflex artery occlusion with thrombus was noted and a stent placed successfully. Subsequent laboratory studies demonstrated positive troponin value with the typical rise and fall pattern of AMI. Echocardiography revealed posterior wall hypokinesis. The patient did well without complication and was discharged on hospital day 3 with a diagnosis of uncomplicated APMI; at follow-up, he was pain-free and feeling well.
