- Clinical Technology
- Adult Immunization
- Hepatology
- Pediatric Immunization
- Screening
- Psychiatry
- Allergy
- Women's Health
- Cardiology
- Pediatrics
- Dermatology
- Endocrinology
- Pain Management
- Gastroenterology
- Infectious Disease
- Obesity Medicine
- Rheumatology
- Nephrology
- Neurology
- Pulmonology
Hereditary Breast Cancer Syndromes: When and Why to Screen and What to Say When You Don't
A healthy 50-year-old woman walks into your office; she is concerned about her risk of breast cancer because right-sided breast cancer was diagnosed in her mother at age 55. She is of Caucasian ancestry and has no other family members with breast, ovarian, or prostate cancer. She has read the news about an actress who had a “cancer gene” and ended up having prophylactic mastectomies. She is very concerned about her risk of developing breast cancer and wants to be “tested.”
A healthy 50-year-old woman walks into your office; she is concerned about her risk of breast cancer because right-sided breast cancer was diagnosed in her mother at age 55. She is of Caucasian ancestry and has no other family members with breast, ovarian, or prostate cancer. She has read the news about an actress who had a “cancer gene” and ended up having prophylactic mastectomies. She is very concerned about her risk of developing breast cancer and wants to be “tested.”
What do you tell her?
Although a family history of breast or ovarian cancer is common in women in whom either condition is diagnosed, a germline (inherited) mutation is identified in fewer than 10% of women with breast cancer. When an underlying genetic defect is present, most cases will be due to breast cancer susceptibility genes (BRCA1 and BRCA2). Both genes are tumor suppressor genes involved in double-stranded DNA repair. Less commonly, other hereditary cancer syndromes such as mutations in TP53 (Li-Fraumeni syndrome) and PTEN (Cowden syndrome) predispose to hereditary breast cancer.1
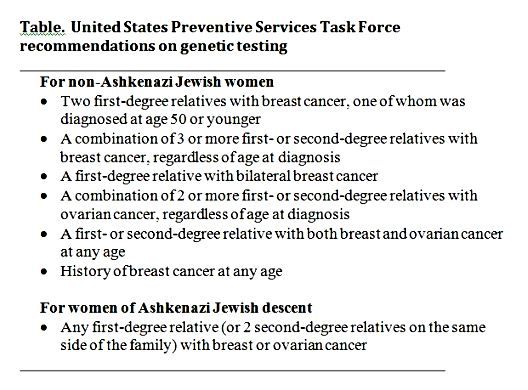
A thorough history is the key factor in determining whether genetic testing should be offered. The United States Preventive Services Task Force (USPSTF) on genetic testing recommends testing based on certain criteria (Table). Features in the history that increase the risk of hereditary breast cancer syndromes include the number of affected relatives, the degree of the relationship between the proband and the affected individual, young age at diagnosis, and multiple primary cancers. The presence of breast cancer in any male relatives should alert clinicians to the possibility of a hereditary breast cancer syndrome and requires testing. Women of Ashkenazi Jewish descent have a higher risk and thus a lower threshold for testing2,3 (Table). It is important to note that these recommendations do not apply to women with a family history of breast or ovarian cancer with known BRCA deleterious mutations.
Financial, emotional cost
Genetic testing is expensive and involves a lengthy process that requires pre- and post-test genetic counseling. Routine testing could also result in adverse ethical, legal, and social consequences. Interventions such as prophylactic mastectomies, chemoprevention, or intensive screening could also have adverse effects. The USPSTF recommends against routine referral for genetic counseling or routine testing for women whose family history is not associated with an increased risk for BRCA1 and BRCA2 deleterious mutations.2
This patient’s initial family history is not suggestive of high risk. Despite having a positive history in her mother who had unilateral breast cancer, the patient’s risk is still not significantly higher than that in the general population. If an in-depth history reveals no other affected family members, then it would be appropriate to counsel the patient that her risk is not high enough to warrant BRCA testing and to explain the risks associated with unnecessary testing. Because she is 50 years old, it would be appropriate to counsel her that she should start annual or biannual mammograms per USPSTF guidelines.4
As public awareness increases about hereditary breast cancer syndromes, primary care physicians should be familiar with and well versed in the application of these criteria for genetic testing in order to appropriately guide patients and their families.
References
1. Foulkes WD. Inherited susceptibility to common cancers. N Engl J Med. 2008;359:2143-2153.
2. US Preventive Services Task Force. Genetic risk assessment and BRCA mutation testing for breast and ovarian cancer susceptibility: recommendation statement. Ann Intern Med. 2005;143:355-361.
3. US Centers for Disease Control and Prevention. Public Health Genomics. Breast and Ovarian Cancer and Increased Risk Family History Patterns. Accessed July 26, 2013.
4. US Preventive Services Task Force. Screening for Breast Cancer. Accessed July 26, 2013.
