- Clinical Technology
- Adult Immunization
- Hepatology
- Pediatric Immunization
- Screening
- Psychiatry
- Allergy
- Women's Health
- Cardiology
- Pediatrics
- Dermatology
- Endocrinology
- Pain Management
- Gastroenterology
- Infectious Disease
- Obesity Medicine
- Rheumatology
- Nephrology
- Neurology
- Pulmonology
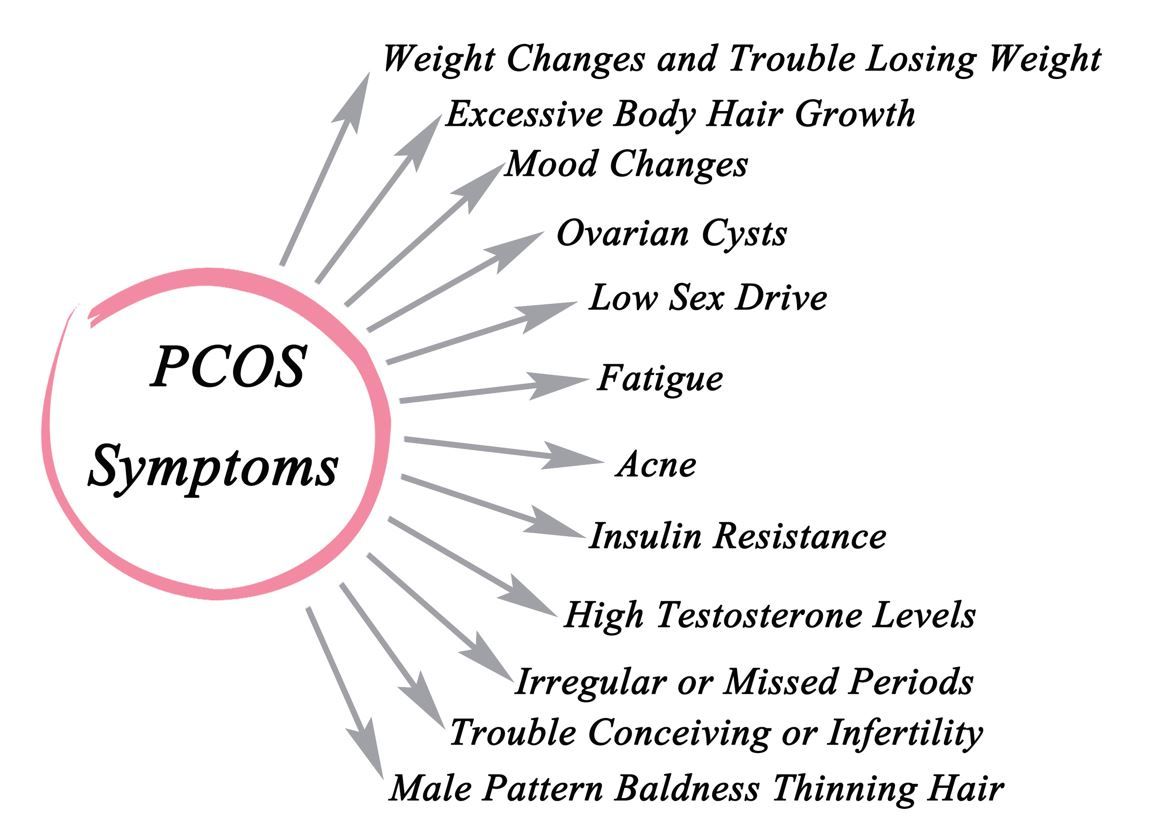
GLP1-RAs Superior to Metformin for CVD Risk Reduction in Women with PCOS, Large Study Finds
The findings support the potential cardiovascular advantages of the GLP-1RA class in women with PCOS, a population already at increased cardiometabolic risk.
Glucagon-like peptide-1 receptor agonists (GLP-1RA) significantly reduced the risk of cardiac arrhythmia and thrombotic disorders by a mean 19% compared with metformin in women with polycystic ovary syndrome (PCOS), according to study findings of a study presented at the 2025 American College of Obstetricians and Gynecologists Annual Clinical & Scientific Meeting, May 16-18, 2025, in Minneapolis, MN.
©Dmitry/stock.adobe.com
The real-world multicohort analysis, which drew data from more than 60 US health care institutions, enrolled girls and women aged 12 years and older diagnosed with PCOS and prescribed at least 2 doses of either a GLP-1RA or metformin between May 1, 2005, and December 31, 2021.
GLP-1RA are recommended by the American Diabetes Association as first line treatment for type 2 diabetes based on evidence of their pleiotropic cardiometabolic benefits. Effects of the class on PCOS are less well studied, according to the study abstract. The current study was designed to compare the effects of GLP-1RA on cardiovascular events in women with PCOS to those of metformin, “an active comparator with known cardiometabolic benefits,” according to presenting author Ting-Wei Ernie Liao, a postdoctoral associate at the Broad Institute of MIT and Harvard, and colleagues.
Researchers observed study participants for 3 years after they initiated treatment with one of the medications. Following 1:1 propensity score matching on body mass index, comorbidities, lipid profiles, Hb A1C, and concomitant medications, Liao and colleagues found that treatment with a GLP-1RA was associated with a 17% lower risk of arrhythmia (HR 0.83; 95% CI, 0.75–0.91) and a 22% lower risk of thrombotic disorders (HR 0.78; 95% CI, 0.68–0.90) compared to metformin therapy.
They also reported trends toward lower risk among participants treated with GLP-1RA for cerebrovascular events (HR 0.88; 95% CI, 0.77–1.01), ischemic heart disease (HR 0.97; 95% CI, 0.83–1.13), inflammatory heart disease (HR 0.97; 95% CI, 0.74–1.26), and major cardiovascular events overall (HR 0.93; 95% CI, 0.83–1.03). None of the differences, however, reached statistical significance, the researchers wrote.
The findings support potential cardiovascular advantages of GLP-1RA beyond glycemic control in the PCOS population—a group already at elevated cardiometabolic risk. Although the etiology of PCOS is not completely understood, pathogenesis commonly involves insulin resistance and subsequent cardiometabolic abnormalities, including dyslipidemia, hypertension, glucose intolerance, diabetes, and metabolic syndrome, all of which place women at increased risk for cardiovascular disease.2 Reflecting outcomes of the current study and the authors’ conclusions, well-known preventive cardiologist and women’s health advocate Erin Michos, MD, of the Johns Hopkins Ciccarone Center for the Prevention of Cardiovascular Disease, Baltimore, MD, writes in a separate study, “Opportunities to implement CVD prevention strategies in these women [with PCOS] should be given high priority.”2
Check out all the Patient Care ACOG 2025 coverage.
