- Clinical Technology
- Adult Immunization
- Hepatology
- Pediatric Immunization
- Screening
- Psychiatry
- Allergy
- Women's Health
- Cardiology
- Pediatrics
- Dermatology
- Endocrinology
- Pain Management
- Gastroenterology
- Infectious Disease
- Obesity Medicine
- Rheumatology
- Nephrology
- Neurology
- Pulmonology
Dyslipidemia: Rational Use of the Statins
Although the cardiovascular death ratehas declined in the United States, thenumber of hospitalizations for cardiacdisease has not. The improvement incare has been offset by an increase inthe number of older Americans. By2050, more than 100 million Americanswill be 60 years of age or older,and about 30 million will be older than80 years.
Although the cardiovascular death rate has declined in the United States, the number of hospitalizations for cardiac disease has not. The improvement in care has been offset by an increase in the number of older Americans. By 2050, more than 100 million Americans will be 60 years of age or older, and about 30 million will be older than 80 years.
As the number of older persons rises, clinicians will see more patients with chronic conditions-such as obesity, diabetes mellitus, and uncontrolled hypertension-that increase the risk of coronary heart disease (CHD). These risk factors have been well established by the Framingham Study1 and other epidemiologic reports. The combination of increased caloric intake and reduced physical activity that has become prevalent in our society will also contribute to a higher incidence of the metabolic syndrome-a condition whose manifestations include increased abdominal girth, low levels of high-density lipoprotein (HDL) cholesterol, hypertension, and elevated blood glucose and triglyceride levels.
All of these factors and others suggest that we must actively pursue strategies-such as global risk assessment and the aggressive control of modifiable risk factors-to protect our patients from CHD, which continues to be the leading cause of death in this country. In recent years, aggressive therapy has resulted in a major improvement in the outlook for patients at risk. Yet many of these persons fail to achieve the treatment goals set forth by the National Cholesterol Education Program (NCEP).2 Moreover, many asymptomatic patients at increased risk who would benefit from treatment are not receiving it.
In this article I highlight data from important clinical trials that demonstrate the benefits of lipid-lowering therapy. I also discuss the major causes of undertreatment.
ROLE OF STATINS IN REDUCING CHD RISK
Cardiovascular risk assessment must include intensive scrutiny of a patient's lipid profile, with particular attention to low-density lipoprotein (LDL) cholesterol, the most atherogenic cholesterol (Table 1). Although very high LDL levels secondary to genetic hyperlipidemia present a significant risk, this condition is rare. In fact, initial coronary events occur much more frequently in persons with serum LDL cholesterol levels between 130 and 160 mg/dL (ie, values below those that warrant drug therapy according to the NCEP guidelines).
The rationale for lowering elevated LDL cholesterol levels is supplied by a host of double-blind, placebo-controlled trials that have demonstrated a reduction in primary and secondary cardiac events in patients who are given HMG-CoA reductase inhibitors (statins)
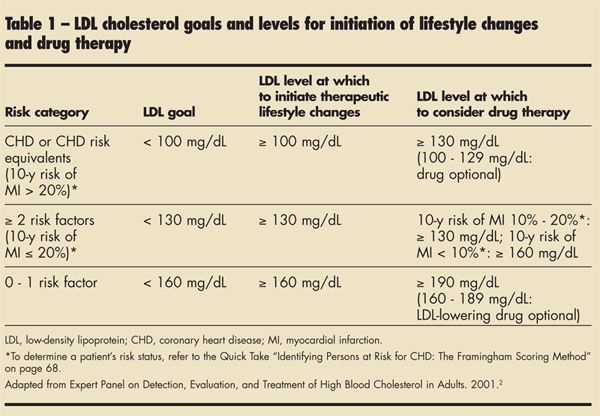
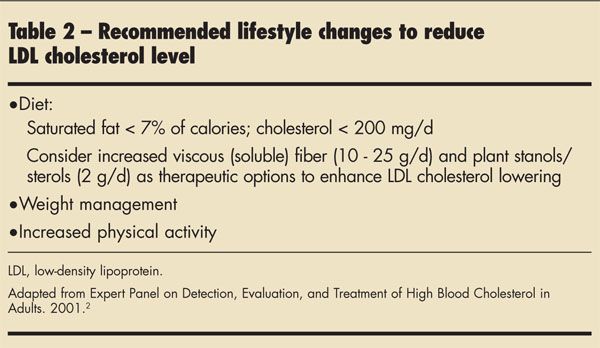
Primary prevention. The degree of absolute risk-the likelihood that CHD will develop within a specific period- guides the intensity of primary prevention efforts. Patients are considered at high risk if the probability that they will suffer a myocardial infarction (MI) in the next 10 years is greater than 20%. According to the NCEP guidelines, risk factors in addition to elevated LDL cholesterol levels include hypertension, cigarette smoking, low levels of HDL cholesterol, CHD, and CHD risk equivalents. The latter group consists of other clinical forms of atherosclerotic disease-such as peripheral arterial disease, previous abdominal aortic aneurysm, and symptomatic carotid artery disease-and diabetes. The NCEP guidelines emphasize that although persons at higher risk are candidates for drug therapy, lifestyle changes are the foundation of primary prevention. The NCEP recommendations are summarized in Table 2.
Two major randomized, doubleblind, placebo-controlled trials evaluated the effectiveness of statin therapy in primary prevention. In the West of Scotland Coronary Prevention Study (WOSCOPS), pravastatin was compared with placebo in men who had elevated LDL cholesterol levels and no known heart disease.3 In the Air Force/Texas Coronary Atherosclerosis Prevention Study (AFCAPS/ TexCAPS), lovastatin was compared with placebo in adults with average total cholesterol and low levels of HDL cholesterol.4 Hospital admission for unstable angina was considered an endpoint cardiac event.
Both studies demonstrated a significant reduction in first cardiacevents in otherwise healthy persons treated with statins. Neither trial was powered to provide statistically significant evidence of a mortality benefit because the number of deaths was small.
Secondary prevention. A host of studies have demonstrated the value of reducing the level of LDL cholesterol in patients with established CHD and hyperlipidemia. The Scandinavian Simvastatin Survival Study (4S) examined data from 4444 patients with known CHD who were randomized to drug therapy or placebo and followed for 5 years.5 The results showed a dramatic reduction in cardiac deaths, stroke, hospitalizations, and need for revascularization in the treated group. This was the first major study to demonstrate a statin-associated reducreduction in all-cause mortality in patients with CHD who had high serum LDL cholesterol. Most previous trials were not powered to demonstrate a difference in an infrequent event end point.
The Cholesterol and Recurrent Events (CARE) trial followed 4159 men and women with average cholesterol levels who had had an acute MI.6 They were randomly assigned to pravastatin or placebo and followed for 5 years. There was a significant reduction in the incidence of cardiovascular events and stroke in the treated patients. Lowering the LDL cholesterol below 124 mg/dL did not seem to provide additional benefits.
Both 4S and CARE recruited patients several months after they had recovered from an acute MI. These studies excluded patients in the immediateperiod after an acute event, when recurrent ischemia and death are most likely to occur.
Subsequently, the Myocardial Ischemia Reduction With Aggressive Cholesterol Lowering (MIRACL) study randomized 3086 patients with acute coronary syndrome (ACS) within 24 to 96 hours after hospital admission to either atorvastatin, 80 mg/d, or placebo with a 16-week follow-up.7 The treated group had a lower risk of ischemia requiring hospitalization and had fewer strokes; there were, however, no significant differences in risk of death, nonfatal MI, or cardiac arrest between the groups.
The value of statin therapy is not limited to patients with acute MI or even unstable ACS. In the Atorvastatin Versus Revascularization Treatment (AVERT) trial, 341 patients with stable coronary artery disease, relatively normal left ventricular function, asymptomatic or mild to moderate angina, and an LDL cholesterol level of at least 115 mg/dL who were referred for percutaneous transluminal coronary angioplasty (PTCA) were randomized to atorvastatin, 80 mg/d, or PTCA followed by usual care.8
After 18 months, the incidence of ischemic events-as well as PTCA and coronary artery bypass graft procedures and hospitalizations for worsening angina-was lower in the atorvastatin group. There was no mortality benefit for PTCA. After adjustment for interim analysis, the results just missed statistical significance. At the end of the study, more patients who had undergone PTCA reported improvement in angina; however, these patients were more likely to have started or increased antianginal medication. The researchers concluded that in low-risk patients with stable coronary artery disease, aggressive lipid-lowering therapy was at least as effective as PTCA and usual care in reducing the incidence of ischemic events.
TREATMENT PEARLS AND PITFALLS
Titration. The appropriate starting dose of a statin is a practical concern, primarily because of the difficulty of titration in office practice. Many primary care physicians, especially those who labor under the constraints of managed care, may not have the time for the increased number of visits required. In addition, patients-many of whom have no symptoms-may be reluctant to invest the time (and money) needed for return visits. Some clinicians are uneasy about the possibility of side effects as the dosage is increased.
The ideal is to achieve target lipid levels with the starting dose of the statin; however, this does not always occur. No single starting dose can be recommended for all patients. Each patient's needs must be taken into account and the regimen individualized accordingly. Measure lipid levels every 6 to 12 weeks, and adjust the dosage based on the patient's response to therapy.
A number of studies have compared the relative efficacy of the various statins across a typical patient cohort. The CURVES trial compared the efficacy of daily starting doses of 5 agents-atorvastatin, 10 mg; simvastatin, 10 mg; pravastatin, 20 mg; lovastatin, 20 mg; and fluvastatin, 20 mg- in patients with hypercholesterolemia for 8 weeks. The mean reductions in LDL cholesterol levels were, respectively, 38%, 28%, 24%, 29%, and 17%. The CURVES study also compared these drugs during titration up to 80 mg for atorvastatin and lovastatin and up to 40 mg for fluvastatin, pravastatin, and simvastatin.9 Atorvastatin at doses of 10, 20, and 40 mg produced greater reductions in LDL cholesterol levels than the milligram equivalent doses of the other agents.
Since the CURVES study was published, the usual starting doses of several statins have been changed to achieve maximum lipid-lowering effects as early as possible. For example, a daily starting dose of 20 mg of simvastatin is now generally recommended, as is an 80-mg dose of long-acting fluvastatin.
Failure to achieve therapeutic goals. A number of studies have demonstrated that goal LDL cholesterol values are achieved relatively infrequently in clinical practice. For example, the Lipid Treatment Assessment Project (L-TAP), a study of the outpatient treatment of dyslipidemia, revealed that only 18% of patients with CHD had achieved the NCEP goal of 100 mg/dL.10 In the Heart and Estrogen/Progestin Replacement Study (HERS), a randomized trial of estrogen plus progesterone for secondary prevention of CHD in women, only 10% of patients achieved an LDL cholesterol goal of 100 mg/dL.11Discharge after MI without therapy. Despite the prodigious evidence that supports the value of lipid-lowering therapy in secondary prevention, most patients who have had an acute MI leave the hospital without statin therapy. In one recent analysis, discharge medication data were collected for 138,000 patients with acute MI from 1470 hospitals. Fewer than one third (31.7%) of the patients were given a prescription for a lipid-lowering drug at discharge.12 The benefits of in-hospital initiation are well established (Box).13,14
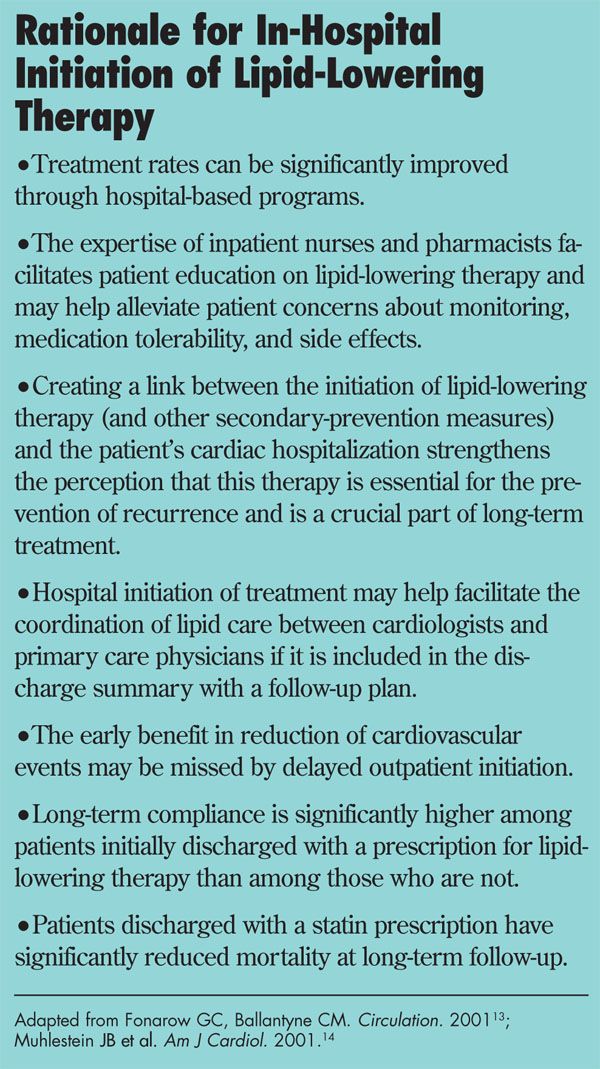
An observational analysis of data from 2 major clinical trials compared mortality among 3653 patients admitted to the hospital with symptomatic CHD who were discharged with lipid-lowering therapy with mortality among 17,156 discharged patients without such therapy.15 The results included a 50% reduction in the death rate at both 30 days and 6 months among the treated patients.
Undertreatment of elderly patients. Many patients who previously had been considered too old for pharmacologic therapy now regularly undergo cardiac revascularization at the first episode of symptomatic ischemic disease. The NCEP guidelines suggest that for primary prevention, lifestyle changes are the first line of therapy for older persons, but that LDL-lowering drugs can be considered when patients are at high risk. The results of secondary prevention trials of statin therapy that included persons aged 65 to 75 years showed that treatment was associated with significant risk reduction.16Hazards of statin/fibric acid therapy. The use of a statin in combination with a fibric acid derivative increases the risk of rhabdomyositis and should be restricted to patients at very high risk; these patients are best referred to specialists. The recent withdrawal of cerivastatin from the market was prompted by an increase in the incidence of rhabdomyositis among patients treated with high doses of this agent or with a combination of cerivastatin and fibric acid derivatives.
OTHER POTENTIAL BENEFITS OF STATINS
The statins may have other benefits besides the effects of lowering LDL cholesterol levels. There is compelling in vivo evidence for direct inhibition of acute and chronic inflammatory conditions characterized by the infiltration of polymorphonuclear leukocytes.17 This is important because of the concept of "vulnerable plaque," in which disruption initiates a cascade of events leading to ACS, acute MI, or sudden death. The features of vulnerable plaque include:
- A large, predominantly acellular lipidrich core.
- A fibrous cap with focal areas of thinning and reduced smooth muscle density and collagen content.
- Inflammatory cell infiltration at the shoulders of the lesion.
Anti-inflammatory effects. The anti-inflammatory effects of the statins may explain some of the reduction in cardiac events seen in clinical trials. Changes in the oxidation-sensitive mechanisms in the arterial wall, effects on nitric oxide synthesis, and modulation of intracellular signaling pathways may all play a role.
Coronary atherosclerotic disease. In a recent study of the effect of fluvastatin on the progression of coronary arteriosclerotic lesions measured by serial computerized angiograms, the reduction in the narrowing of coronary lumen associated with treatment occurred irrespective of baseline LDL cholesterol levels.18 Lipid effects independent of the lowering of LDL cholesterol levels include inhibition of LDL cholesterol oxidation and secretion and inhibition of scavenger receptor expression. Antiatherosclerotic effects include inhibition of migration and proliferation of arterial myocytes, inhibition of macrophage growth, inhibition of metaloproteinase secretion, inhibition of cell adhesion, and increased expression of endothelial nitric oxide synthase.
Possible prophylactic effects. A reduction in the incidence of type 2 diabetes among patients treated with statins has been reported.6 In a small study, simvastatin reduced blood pressure and 24-hour urinary albumin excretion in patients with type 2 diabetes and hypertension.19
Statin use has been associated with a reduction in the risk of dementia. dementia.20 Several studies have suggested that statin use also reduces the risk of stroke.21-23 Other reports have found that statins are associated with a reduction in C-reactive protein levels24 and a decreased risk of deep vein thrombosis.25 Some experts recommend statins as the drug of first choice for reducing cardiovascular risk in women with established CHD.26
FUTURE METHODS OF ASSESSING CHD RISK
A potentially important effect of fluvastatin on QT dispersion was recently reported.27 In a study of patients with hypercholesterolemia, QT interval dispersion (QTd) decreased after treatment with fluvastatin. It has been suggested that analysis of QTd might be used as a noninvasive method of evaluation of the risk of sudden death in patients with CHD.
Sophisticated techniques to help evaluate the treatment of dyslipidemia are emerging rapidly. The cholesterol ester transfer protein (CETP) has a central role in the metabolism of HDL cholesterol and may therefore alter susceptibility to atherosclerosis. A recent study designed to assess the regression of coronary atherosclerosis evaluated the polymorphisms of the B1 variant of the CETP gene.28 The 807 male participants-all of whom had angiographically documented coronary atherosclerosis-were randomly assigned to treatment with pravastatin or placebo. The B1 variant of the CETP gene was associated with both higher plasma CETP concentrations and lower HDL cholesterol levels.
The study showed that pravastatin therapy slowed the progression of atherosclerosis in B1B1 carriers but not in B2B2 carriers (who represented 16% of the patients taking pravastatin). The presence of the B1 variant appears to predict whether men with CHD will benefit from treatment with pravastatin to help delay the progression of atherosclerosis.
Other investigations have produced a single blood test that can identify 35 different cardiovascularrelated gene variants. Eventually, gene testing will predict CHD risk with high accuracy.
