- Clinical Technology
- Adult Immunization
- Hepatology
- Pediatric Immunization
- Screening
- Psychiatry
- Allergy
- Women's Health
- Cardiology
- Pediatrics
- Dermatology
- Endocrinology
- Pain Management
- Gastroenterology
- Infectious Disease
- Obesity Medicine
- Rheumatology
- Nephrology
- Neurology
- Pulmonology
Choking and Chest Tightness: Asthma or Something Else?
A 37-year-old man recently was diagnosed with asthma and prescribed a dry-powder inhaler. He says it's not working and actually making his symptoms worse. What's wrong?
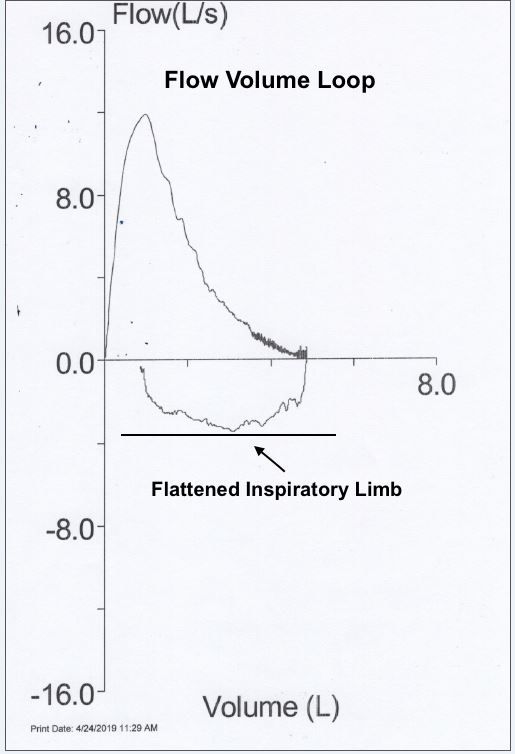
Figure. Flow loop volume tracing (please click to enlarge)
History of present illness
A 37-year-old man presents for evaluation after choking at a bar-b-que; he was administered the Heimlich maneuver, and then taken to a local emergency department.
Physical examination findings were unremarkable; chest x-ray was normal, and serology results were negative. He felt better after nebulizer treatments with albuterol and a dose of IV methylprednisolone. He was diagnosed with asthma and prescribed a dry powder inhaler.
Since the episode 2 weeks ago, he says he has been frequently experiencing a choking sensation and chest tightness. He explains that using the inhaler seems to make the symptoms worse. Review of systems was otherwise negative.
- Past medical history: Hair loss, hypercholesterolemia, low back pain, and gastroesophageal reflux disease (GERD).
- Past surgical history: Nasal septoplasty and lumbar spine microdiscectomy.
- Current medications: Rosuvastatin 10 mg dialy, finasteride 1 mg daily.
- Allergies: No environmental or medication allergies.
- Social history: He works as a real estate agent and has no recent travel or obvious exposures. He has never smoked tobacco and drinks small amounts of alcohol. He works out regularly by swimming and does not experience symptoms while in the pool.
Vital signs, examination, pulmonary function testing
Vital signs
- Height: 69 in; weight: 159 lbs
- BMI: 23.48
- Oxygen: 98% on room air
- Temperature: 98 F
- Heart rate: 107 beats/min
- Respiration: 15 breaths/min
- BP (sitting): 112/80 mm Hg (right upper arm)
- Pulse (sitting): 107 beats/min; rhythm, regular
Examination
- Constitutional: general appearance, no apparent distress
- Eyes, ENT, Neck: WNL
- Respiratory: respiratory effort, normal; auscultation of lungs, clear to auscultation bilaterally
- Cardiovascular: Auscultation of heart, regular rate and rhythm, no rub, murmur, or gallop
- Gastrointestinal: abdomen, soft with slight epigastric tenderness
Pulmonary function testing
The numeric data obtained on pulmonary function testing was normal, ie values for spirometry, maximum voluntary ventilation, lung volumes, and diffusing capacity were all normal. There was no response to bronchodilator. However the inspiratory limb of the flow volume loop was flattened (Please see Figure above; click to enlarge for detail).
What diagnosis does this suggest to you?
Please click here for answer and discussion.
The flattened inspiratory limb of the flow volume loop suggests vocal cord dysfunction (see Figure).
Diagnosis
The patient was diagnosed with vocal cord dysfunction (VCD). VCD is a term that refers to inappropriate adduction of the vocal cords during inhalation and sometimes exhalation.1 The diagnosis was based on the patient’s presenting complains, negative physical examination, normal chest x-ray, and specific pattern on the flow volume loop. Another pertinent detail is that the cool mist of a nebulizer improved his symptoms while the dry powder of an asthma inhaler triggered them. Also, he did not experience symptoms while swimming because the water vapor at the water’s surface soothes the vocal cords during exercise.
Discussion
VCD often mimics asthma. The lack of wheezing in this case and poor response to the dry powder inhaler were a clue that the patient did not have classic asthma. In a review of 1020 patients, Morris and Christopher2 found that VCD symptoms vary widely and common complaints included air hunger, choking sensation, chest tightness, difficulty swallowing, globus, intermittent aphonia or dysphonia, neck or chest retractions, fatigue, and throat clearing. Many of the sensations can elicit fear and panic.2
Triggers are not always identified and episodes are often brief and end abruptly. Self-reported triggers include upper respiratory infections, irritant exposures, laughing, talking, singing, acid reflux, exercise, postnasal drip, strong emotions, and odors.3,4
After the diagnosis was explained, the patient admitted during further questioning an increase in gastroesophageal (GERD) symptoms. He also described chronic anxiety and 2 to 3 episodes per week of choking and panic.
Treatment, outcome, take home points
Treatment
Treatment included education, medication management, and counseling. The education included information on VCD, GERD, the benefits of swimming, and appropriate diet. Medication management included discontinuation of the dry powder inhaler and addition of ranitidine 150 mg twice daily for GERD. Counseling consisted of referral to a psychologist to improve coping mechanisms.
Outcome
At follow-up 6 weeks later, the patient reported improvement. He estimated that the number of episodes was decreased by 50%. At the 12-week follow-up visit, VCD symptoms were gone.
Take Home Points
- VCD can mimic asthma
- Dry powder inhalers make symptoms worse
- Values for pulmonary function testing are normal
- The flow volume loop has a flattened inspiratory limb
- VCD triggers are similar to those for asthma
- The underlying cause typically requires a multidisciplinary treatment approach
Dr Schroeder is Clinical Instructor of Medicine at UCLA, David Geffen School of Medicine and Clinical Chief of Pulmonary and Critical Care Medicine, Emeritus, at Cedars-Sinai Medical Center.
REFERENCES
1. Hoyte FC. Vocal cord dysfunction. Immunol Allergy Clin North Am. 2013;33:1-22.
2. Christopher KL, Wood RP 2nd, Eckert RC, et al. Vocal cord dysfunction presenting as asthma. N Engl J Med. 1983;308:1566-70.
3. Andrianopoulos MV, Gallivan GJ, Gallivan KH. PVCM, PVCD, EPL, and irritable larynx syndrome: what are we talking about and how do we treat it? J Voice. 2000; 14:607-18.
4. Morrison M, Rammage L, Emami AJ. The irritable larynx syndrome. J Voice. 1999;13:447-55.
