- Clinical Technology
- Adult Immunization
- Hepatology
- Pediatric Immunization
- Screening
- Psychiatry
- Allergy
- Women's Health
- Cardiology
- Pediatrics
- Dermatology
- Endocrinology
- Pain Management
- Gastroenterology
- Infectious Disease
- Obesity Medicine
- Rheumatology
- Nephrology
- Neurology
- Pulmonology
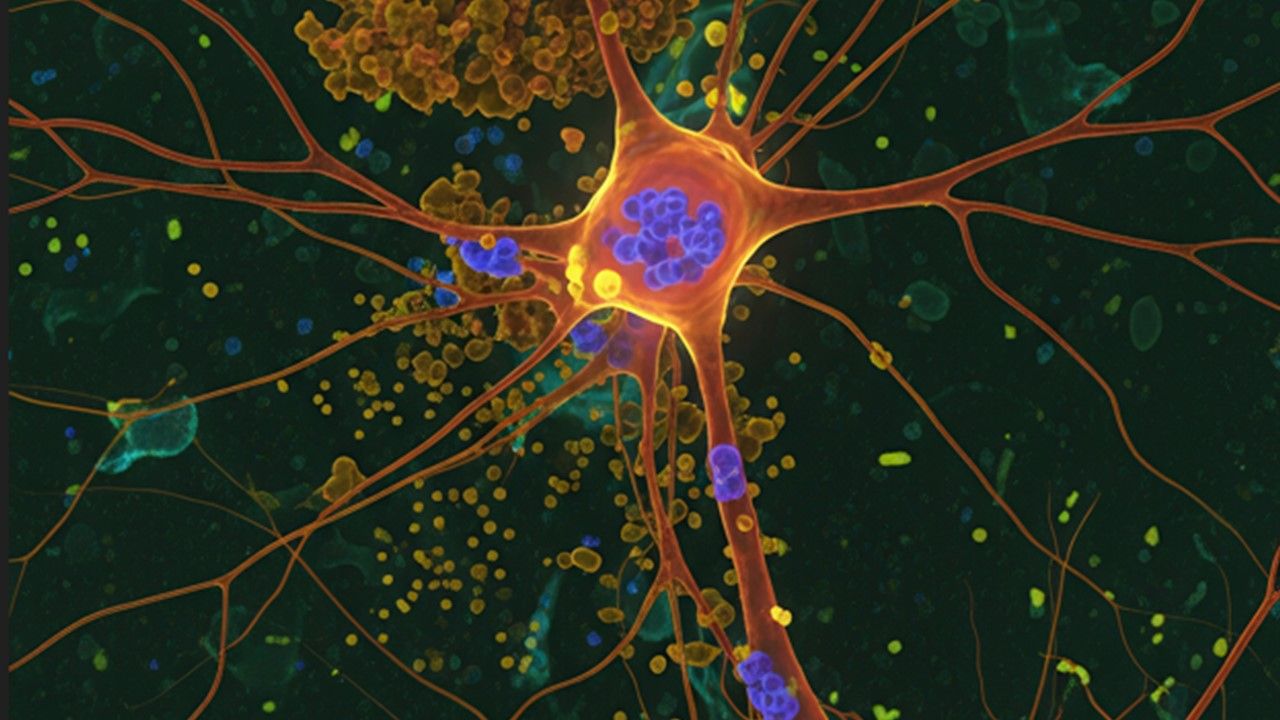
Alzheimer's Association Releases First Clinical Guideline on Use of Blood-Based Biomarker Tests
The guideline is the first in a series that will focus on diagnosis, treatment, and care of Alzheimer disease and all other dementias, according to the association.
The Alzheimer’s Association has released its first-ever clinical practice guideline for the use of blood-based biomarker (BBM) tests to help diagnose Alzheimer disease (AD) in individu als with cognitive impairment.1 The guideline, announced at the Alzheimer’s Association International Conference 2025, outlines when and how to use BBM tests, such as those measuring abnormal amyloid beta (Aβ) or tau proteins, in specialized memory-care settings.1
©ryandi/stock.adobe.com
It provides 2 evidence-based recommendations:
- that BBM tests with 90% or greater sensitivity and 75% or greater specificity may be used as a triaging tool to rule out AD pathology
- that BBM tests with 90% or greater sensitivity and 90% or greater specificity may be used as a substitute for confirmatory tests such as PET imaging or cerebrospinal fluid (CSF) analysis
The guideline is the first in a series of clinical practice guidelines for the "diagnosis, treatment, and care of AD and all other dementia," according to a statement from the Alzheimer's Association.1
“This is a pivotal moment in Alzheimer’s care,” Maria C. Carrillo, PhD, chief science officer at the Alzheimer’s Association and a co-author of the guideline, said in the statement. "For the first time, we have a rigorously evidence-based guideline that empowers clinicians to use blood biomarker tests confidently and consistently. Adoption of these recommendations will lead to quicker, more accessible, more accurate diagnoses—and better outcomes for individuals and families affected by Alzheimer’s.”
BBMs represent a promising, accessible, and potentially cost-effective advance in AD diagnostics, but their integration into clinical practice remains complex, an international group of experts said in a review of challenges in The Lancet: Healthy Longevity.2 For specialty care, including memory clinics, adoption hinges on establishing diagnostic accuracy and demonstrating impact on clinician confidence and patient management. For primary care, where experience with AD BMMs is minimal, challenges include educating frontline providers and developing clear implementation protocols, the researchers wrote.2 Widespread use will also require standardization of assay conditions and attention to confounders such as comorbidities and population diversity. Despite these hurdles, the group asserts, BBMs have the potential to improve diagnostic precision and streamline referrals, which translate in to earlier intervention in AD.2
The Alzheimer's Association guideline authors echo these thoughts and add other caveats, cautioning that not all BBM tests are equivalent, and many commercially available options do not yet meet the performance thresholds defined by the panel. “Not all BBM tests have been validated to the same standard or tested broadly across patient populations and clinical settings, yet patients and clinicians may assume these tests are interchangeable,” Rebecca M. Edelmayer, PhD, vice president of scientific engagement at the Alzheimer’s Association and also a co-author, said. “This guideline helps clinicians apply these tools responsibly, avoid overuse or inappropriate use, and ensure that patients have access to the latest scientific advancements.”1
This set of recommendations is intended for clinicians working in secondary or tertiary care settings and are based on a systematic review of 49 observational studies that evaluated 31 different BBM tests. The Alzheimer’s Association opted not to endorse specific commercial tests but used a brand-agnostic, performance-based approach to minimize bias. The guideline is the first evidence-based guideline in the AD category developed using the GRADE (Grading of Recommendations Assessment, Development and Evaluation) methodology to ensure transparency and scientific rigor. BBMs evaluated in the guideline included plasma phosphorylated tau (p-tau217, %p-tau217, p-tau181, p-tau231) and Aβ 42/40 ratio.1
Context is Essential
A Good Practice Statement within the guideline emphasizes that BBM tests should not be ordered before a comprehensive clinical evaluation and must be interpreted in the context of the individual's overall clinical presentation. The Alzheimer’s Association plans future guidelines addressing cognitive assessment tools, clinical implementation of staging criteria and treatment, and prevention of dementia. All guidelines will be made available through ALZPro, the Association’s new centralized resource hub for dementia professionals.1
References
Alzheimer's Association releases its first clinical practice guideline for blood-based biomarker tests. News release. Alzheimer's Association. July 30, 2025. Accessed July 30, 2025. https://aaic.alz.org/releases-2025/clinical-practice-guideline-blood-based-biomarkers.asp
Scholl MS, Verberk IMW, del Campo M, et al. Challenges in the practical implementation of blood biomarkers for Alzheimer’s disease. Lancet Healthy Longev. 2024;5(10):100630. doi:10.1016/ j.lanhl.2024.07.013
