- Clinical Technology
- Adult Immunization
- Hepatology
- Pediatric Immunization
- Screening
- Psychiatry
- Allergy
- Women's Health
- Cardiology
- Pediatrics
- Dermatology
- Endocrinology
- Pain Management
- Gastroenterology
- Infectious Disease
- Obesity Medicine
- Rheumatology
- Nephrology
- Neurology
- Pulmonology
Allergic Rhinitis
Physical clues to allergic rhinitis include the allergic crease on the dorsum of the nose and allergic "shiners" or periorbital ecchymosis.
This teenager has pressed her right palm against the tip of her nose (Figure, top), pushing it toward her mid-face so [[{"type":"media","view_mode":"media_crop","fid":"31374","attributes":{"alt":"Allergic salute","class":"media-image media-image-right","height":"278","id":"media_crop_3554928878002","media_crop_h":"0","media_crop_image_style":"-1","media_crop_instance":"3302","media_crop_rotate":"0","media_crop_scale_h":"0","media_crop_scale_w":"0","media_crop_w":"0","media_crop_x":"0","media_crop_y":"0","style":"float: right;","title":" ","typeof":"foaf:Image","width":"161"}}]]as to compress the nose and perhaps widen the external aperture of each naris. This maneuver does not merely wipe away nasal discharge, which would be better accomplished, in the absence of tissue or handkerchief, by the back of the sleeve or worse yet with cupped hand or pincer use of thumb and forefinger. The gesture is called an allergic salute by analogy to raising the hand to mid-face in a military salute, and is a good though not pathognomonic marker of allergic rhinitis, which is confirmed by the history. The salute relieves local nasal itching, can move discharge away, and may ease passage of air through the nose.
One further observes (Figure, bottom) a subtle transverse allergic crease on the dorsum of the nose, a residue of many prior salutes. Faint but definite darkenings of skin beneath each eye constitute mild allergic shiners. In scrutinizing the entire facies, one notes no visible eczema, no discernible local swelling including about the eyelids, nor any ocular discharge. Thus, any associated atopic eczema might be turned up only by personal or family history, or wider examination of skin, especially for dry skin in the elbow or knee flexures. The common association with asthma warrants parallel exploration and monitoring over time.
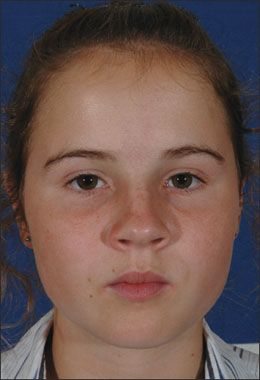
Full-face view shows bright-eyed young person with no edema of lids, no blepharoconjunctivitis, and no chemosis. Mouth is closed, so we can infer that she is nose-breathing.
ALLERGIC RHINITIS: SHINERS
Allergic rhinitis is associated with two other "allergic" signs: Allergic shiners perpetuate the old slang term for a black eye, itself a highly descriptive lay term for periorbital ecchymosis. Black eyes are most closely associated with trauma, typically a punch in the face, but have many other causes.1 The predictive value of this common sign for allergic rhinitis is debated,2,3 which makes sense in that the venous congestion that underlies it-perhaps along with a smidgeon of melanocyte stimulation-can result from any inflammatory process in the periocular tissues, whether allergic or other. However, given that allergic rhinitis is the commonest chronic disorder of children, it is often a safe inference to connect this feature to a history of long-standing "stuffiness" and clear nasal discharge. 4-8 Edema of the lower eyelids often accompanies allergic shiners, but local edema without discoloration will raise other differential diagnoses such as nephrotic syndrome, contact dermatitis, and even the now-rare trichinosis.7
Allergic shiners take time to develop, and a long time to resolve though they may lighten; they should not occur in uncomplicated seasonal allergic rhinitis.
ALLERGIC RHINITIS: CREASES
Allergic creases were first and well described in 1960.8 They consist of darkened or hypopigmented transverse lines that cross the cartilaginous dorsum of the nose, distinct from the momentary blanching of the same skin that occurs just after an allergic salute. Myers8 found that at least 2 years of repetitive allergic salutes was the minimum associated with this enduring mark of repetitive brief crumple-injury to the nasal skin. The same crease can occur after prenatal exposure to cocaine; but facial and neurological abnormalities are so striking in that setting, and the history usually so blatant, that one is unlikely to mistake it for allergic rhinitis.9 The only other published source of this sign is congenital crease of the nasal bridge, which may harbor a mimic of acne within it10; other "nasal crease signs" refer to the inferior columella.11
EXTRAORDINARILY SPARSE LITERATURE
Much has been published about the appearance of the nasal mucosa in allergic rhinitis versus viral illness versus rhinitis medicamentosa, but most clinicians would interpret the total picture and not take this facet as determinative in isolation, regarding the appearance of the nasal mucosa as an unreliable clinical sign.
By contrast, although the "allergic triad" of allergic shiners, allergic salute, and allergic crease is familiar to pediatricians,4,7 allergologists, and otorhinolaryngologists,4-8 internists may not be aware of them-the internist co-author of this paper learned of them 25 years post residency. A PubMed search of the immense database of the US National Library of Medicine, using the terms, in both singular and plural form, "allergic salute OR allergic crease OR allergic shiner" yielded only 31 "hits" in total.2,3,5-7,9-16 (To give an idea of just how few these are, we searched under the name of one of the rarest of neoplasms, "hemangiopericytoma," and found 2769 hits!) Many of the articles named by this search proved altogether off-topic, eg, about triggers of allergy against fish, with no mention of the nose or eye region of humans at all. Some others relate minimally; for instance, a review of the role of leukotrienes merely names the signs as common findings in allergic rhinitis, in the conclusions section of its abstract and not in the body of the article at all.16 Perhaps these signs constitute such familiar "black letter law" to those who see them often, that they have generated minimal discussion in journals.
THE ADENOID FACIES
Happily, this adolescent is free of any trace of the "adenoid facies" of chronic nasal obstruction. That features a gaping mouth due to mouth-breathing, and sagging eyelids giving the correct impression of sleep deprivation related to poor sleep quality. This "adenoid constellation" has become a kind of visual clich in film, popular art, and literature, so that once aware of it, one sees it ever more frequently-fortunately in historical materials more often than in contemporary ones. Allergy could lead to an adenoid facies via chronic nasal obstruction; however, this more commonly occurs with adenoidal hyperplasia. The key element is nasal obstruction that forces mouth-breathing.
Two classic descriptions warrant reprinting: First, how this appearance was viewed in 1894: "Adenoid masses about the size of millet seeds are met with in the vault of the pharynx. . . . In a characteristic case the aspect of a child who suffers from adenoids is peculiar: the expression is vacant, the mouth half open, the face elongated, and the nose narrow. There is noisy breathing, and usually some impairment of hearing"17; this may also have been an early description of the association of adenoid disease with otitis media with effusion.
Second and equally cruel, from an otherwise brilliant 1960 textbook by Kampmeier18: "The adenoid facies, seen especially in children, is characterized by the thin face, pinched nose, highly arched palate, often a receding chin, mouth breathing, and frequently a stupid expression. The abnormalities result from breathing through the mouth because of nasal obstruction." A bit later he adds, "The child who has obstruction from enlarged adenoids and must therefore breathe through his mouth . . . [may have] very small nasal passages."
Part of the utility of reviewing these descriptions is reassurance that our advances usually preempt such a stage, though a subset of cases of allergic rhinitis provide major therapeutic challenges. We have grown kinder: it would be intolerable for any contemporary clinician to describe a medical condition as producing a "stupid" facial expression. However, in 1960 pediatric obstructive sleep apnea was not recognized; Kampmeier's may have been an early description of the cognitive impairment associated with obstructive sleep apnea secondary to adenotonsillar hypertrophy.
NEWEST THERAPEUTIC MEASURES
A discussion of topical and systemic measures, including nasal corticosteroids and newer antihistamines,19 exceeds the scope of this column. However, some promising domains warrant brief mention, eg, a striking hypothesis is that a major milk protein, beta-casomorphin-7, might enter the bloodstream and stimulate excess respiratory gland mucus production in an area of preexisting damage.20 Though there has been controversy about this topic for decades, clinically some children and even adults respond dramatically to a strict dairy/chocolate elimination diet for 4 weeks. Note that our index case had improved on a strict dairy-free diet and had worsening of all symptoms when she consumed dairy products.
Desensitization with sublingual drops is already in widespread use in Europe and appears to augment its symptomatic benefit with disease-modifying properties for allergic rhinitis and asthma.21 Three injections of allergen into inguinal lymph nodes appeared to achieve at least as much desensitization as 54 (!) subcutaneous injections.22 Finally, in adults turbinate surgery can enhance symptom control in many otherwise refractory cases.23
References:
REFERENCES:1. Schneiderman H. Conjunctival and orbital ecchymosis, either spontaneous or from occult trauma. Consultant. 2004;44:93-100.
2. Chen CH, Lin YT, Wen CY, et al. Quantitative assessment of allergic shiners in children with allergic rhinitis. J Allergy Clin Immunol. 2009;123:665-671, 671.e1-671.e6.
3. Kelso JM. How allergic are "allergic shiners"? J Allergy Clin Immunol. 2010;125:276; with author reply, same page.
4. Gentile DA, Michaels MG, Skoner DP. Allergy and immunology. In: Zitelli BJ, Davis HW, eds. Atlas of Pediatric Physical Diagnosis. St Louis: Mosby; 2002:88-90.
5. Fireman P. Therapeutic approaches to allergic rhinitis: treating the child. J Allergy Clin Immunol. 2000;105(6, pt 2):S616-S621.
6. Berger WE. Allergic rhinitis in children: diagnosis and management strategies. Paediatr Drugs. 2004;6:233-250.
7. Valet RS, Fahrenholz JM. Allergic rhinitis: update on diagnosis. Consultant. 2009;49:610-613.
8. Myers WA. The "nasal crease." A physical sign of allergic rhinitis. JAMA. 1960;174:1204-1206.
9. Fries MH, Kuller JA, Norton ME, et al. Facial features of infants exposed prenatally to cocaine. Teratology. 1993;48:413-420.
10. Risma KA, Lucky AW. Pseudoacne of the nasal crease: a new entity? Pediatr Dermatol. 2004;21:427-431.
11. Wright DR, Russi DC, Mancini AJ, et al. The nasal crease sign in segmental facial hemangioma-an early sign of cartilage destruction. Pediatr Dermatol. 2007;24:241-245.
12. Carlson RE, Hering PJ. Allergic shiners. JAMA. 1981;246:835.
13. Marks MB. Allergic shiners. Dark circles under the eyes in children. Clin Pediatr (Phila). 1966;5:655-658.
14. Miri S, Farid R, Akbari H, Amin R. Prevalence of allergic rhinitis and nasal smear eosinophilia in 11- to 15 yr-old children in Shiraz. Pediatr Allergy Immunol. 2006;17:519-523.
15. Leccese C. Giving the allergic salute an honorable discharge. Adv Nurse Pract. 1998;6(5):59-62.
16. Haberal I, Corey JP. The role of leukotrienes in nasal allergy. Otolaryngol Head Neck Surg. 2003;129:274-279.
17. Bury JS. Clinical Medicine: A Manual for the Use of Students and Junior Practitioners. London: Charles Griffin and Company, Ltd; 1894:251.
18. Kampmeier RH. Physical Examination in Health and Disease. 2nd ed. Philadelphia: FA Davis Co; 1960:167, 201.
19. Valet RS, Fahrenholz JM. Allergic rhinitis: update on your therapeutic choices. Consultant. 2010;50:155-160.
20. Bartley J, McGlashan SR. Does milk increase mucus production? Med Hypotheses. 2010;74:732-734.
21. Burastero SE. Sublingual immunotherapy for allergic rhinitis: an update. Curr Opin Otolaryngol Head Neck Surg. 2006;14:197-201.
22. Senti G, Prinz Vavricka BM, Erdmann I, et al. Intralymphatic allergen administration renders specific immunotherapy faster and safer: a randomized controlled trial. Proc Natl Acad Sci U S A. 2008;105:17908-17912.
23. Chen Y-L, Tan C-T, Huang H-M. Long-term efficacy of microdebrider-assisted inferior turbinoplasty with lateralization for hypertrophic inferior turbinates in patients with perennial allergic rhinitis. Laryngoscope. 2008;118:1270-1274.
