- Clinical Technology
- Adult Immunization
- Hepatology
- Pediatric Immunization
- Screening
- Psychiatry
- Allergy
- Women's Health
- Cardiology
- Pediatrics
- Dermatology
- Endocrinology
- Pain Management
- Gastroenterology
- Infectious Disease
- Obesity Medicine
- Rheumatology
- Nephrology
- Neurology
- Pulmonology
AHA/ACC Release Revised Hypertension Clinical Practice Guideline to Reduce CVD Risk
Updates to the 2017 guideline focus on new monitoring strategies, earlier intervention to reduce cognitive decline, improved perinatal care, and refined risk assessment.
Nearly half (46.7%) of US adults have hypertension, defined as blood pressure equal to or greater than 130/80 mm Hg and documented as the leading preventable risk factor for cardiovascular disease (CVD). Hypertension is also a major contributor to kidney disease, complications of pregnancy and childbirth, cognitive decline, and dementia, emphasized authors of a new joint guideline from the American Heart Association (AHA) and the American College of Cardiology (ACC).1
Daniel Jones, MD
The “2025 AHA/ACC Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults,” published August 14 in Circulation, Hypertension, and JACC, revises and updates the 2017 iteration, incorporating updated evidence for use of newer therapies (eg, GLP-1 receptor agonists); discussion of the role of early hypertension treatment to reduce the risk of cognitive decline; and use of the AHA’s PREVENT (Predicting Risk of cardiovascular disease EVENTs) risk calculator to estimate CVD risk.1
“High blood pressure is the most common and most modifiable risk factor for heart disease,” Daniel W. Jones, MD, chair of the writing committee and dean and professor emeritus at the University of Mississippi School of Medicine, said in an AHA statement. “By addressing individual risks earlier and offering more tailored strategies across the lifespan, the 2025 guideline aims to aid clinicians in helping more people manage their blood pressure and reduce the toll of heart disease, kidney disease, type 2 diabetes and dementia.”2
To mitigate the many downstream outcomes associated with elevated blood pressure, the updated AHA/ACC guideline emphasizes the need for earlier treatment to reduce risk, with a focus on lifestyle modification, pharmacotherapy as necessary but for all levels of hypertension, and use of appropriate therapies for concomitant disease.1
Key Changes From 2017
- Use PREVENT CVD risk estimator: Clinicians should use the PREVENT calculator to estimate 10- and 30-year CVD risk in adults aged 30 to 79 years. The tool integrates cardiovascular, kidney, and metabolic health indicators, and includes zip code as a proxy for social drivers of health.
- Early intervention to preserve cognition: Initiate treatment for adults with high blood pressure to target systolic blood pressure <130 mm Hg to reduce risk of cognitive decline and dementia.
- Pregnancy care: Start antihypertensive therapy during pregnancy when blood pressure reaches ≥140/90 mm Hg. Consider low-dose aspirin (81 mg/day) to lower preeclampsia risk in women with chronic hypertension. Continue close monitoring postpartum and measure blood pressure annually in those with pregnancy-related hypertension.
- Expanded lab testing: Perform urine albumin-to-creatinine ratio testing in all adults with hypertension. Broaden screening for primary aldosteronism, including in patients with obstructive sleep apnea and those with stage 2 hypertension.
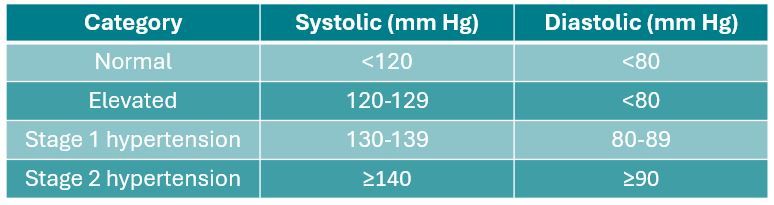
Blood Pressure Classification (unchanged from 2017)
Lifestyle Recommendations
The guideline continues to recommend the AHA's Life’s Essential 8 behaviors as first-line care for all adults:
- Limit sodium to <2,300 mg/day, aiming for 1,500 mg/day.
- Limit alcohol to ≤2 drinks/day for men and ≤1 drink/day for women.
- Maintain or achieve a healthy weight; target ≥5% loss in adults with overweight or obesity.
- Follow a heart-healthy eating pattern, such as DASH.
- Accumulate 75–150 minutes/week of aerobic and/or resistance activity.
- Manage stress through exercise, meditation, breathing techniques, or yoga.
- Use home BP monitoring to confirm diagnosis and guide treatment.
Medication Guidance
The recommended guidance for initiating therapy remains unchanged from the 2017 guideline: For individuals with BP of 140/90 mm Hg or higher (stage 2 hypertension), treatment should begin with 2 medications, ideally in a single combination pill. First-line agents include ACE inhibitors, ARBs, long-acting dihydropyridine calcium channel blockers, and thiazide-type diuretics. Individualizing therapy for patients with comorbidities could include consideration of adding GLP-1 medications in select individuals with hypertension and overweight or obesity.1
“This updated guideline is designed to support health care professionals—from primary care teams to specialists—with the diagnosis and care of people with high blood pressure,” Jones said. “It also empowers patients with practical tools that can support their individual health needs as they manage their blood pressure, whether through lifestyle changes, medications or both.”2
According to the CDC, just two-thirds (68.3%) of adults on treatment for hypertension have their blood pressure controlled to less than 140/90 mm Hg. Fewer than 1 in 4 (22.5%) have reached the guideline recommended target of less than 130/80 mm Hg.2 The disease is more prevalent among men (50.8%) than among women (44.6%) and, regardless of sex, prevalence increases with age, reaching a rate of 71.6% among adults aged 60 years and older.3
Eleven other professional societies, including the American Academy of Physician Associates, the American Association of Nurse Practitioners, the American College of Clinical Pharmacy, the American College of Preventive Medicine, the American Geriatrics Society, the American Medical Association, the American Society of Preventive Cardiology, have co-endorsed the updated guideline.1
References
Jones D, Ferdinand K, Taler S. et al. 2025 AHA/ACC/AANP/AAPA/ABC /ACCP/ACPM/AGS/AMA/ASPC/NMA/PCNA/SGIM guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: A report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. JACC. Published online August 14, 2025. https://doi.org/10.1016/j.jacc.2025.05.007
New high blood pressure guideline emphasizes prevention, early treatment to reduce CVD risk. News release. American Heart Association. August 14, 2025. Accessed August 15, 2025. https://newsroom.heart.org/news/new-high-blood-pressure-guideline-emphasizes-prevention-early-treatment-to-reduce-cvd-risk
Fryar DC, Kit B, Carroll MD, Afful J. Hypertension prevalence, awareness, treatment, and control among adults age 18 and older: United States, August 2021–August 2023. NCHS data brief, No. 511. Hyattsville, MD: National Center for Health Statistics. 2024. https://www.cdc.gov/nchs/products/databriefs/db511.htm
