- Clinical Technology
- Adult Immunization
- Hepatology
- Pediatric Immunization
- Screening
- Psychiatry
- Allergy
- Women's Health
- Cardiology
- Pediatrics
- Dermatology
- Endocrinology
- Pain Management
- Gastroenterology
- Infectious Disease
- Obesity Medicine
- Rheumatology
- Nephrology
- Neurology
- Pulmonology
Addressing a Rash of Allergies: A Photo Essay
Allergic rhinitis and the “allergic triad,” allergy tests for children, allergic asthma, acute urticaria, a lipstick allergy, allergic contact dermatitis of the scalp-these images show a range of common allergic conditions.
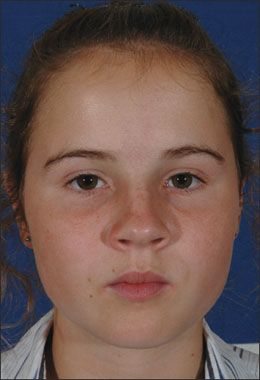
Case 1:
The “allergic triad” consists of allergic shiners, allergic salute, and allergic crease.
This girl shows no edema of lids, no blepharoconjunctivitis, and no chemosis. Her mouth is closed, so it may be inferred that she is nose-breathing. She has pressed her right palm against the tip of her nose, pushing it toward her midface to compress the nose and widen the external aperture of each naris. There are faint darkenings of skin beneath each eye.
She has allergic rhinitis, the most common chronic disorder of children.
Allergic shiners take time to develop and a long time to resolve, although they may lighten. They should not occur in uncomplicated seasonal allergic rhinitis. Their predictive value for allergic rhinitis is debated.
Much has been published about the appearance of the nasal mucosa in allergic rhinitis versus viral illness versus rhinitis medicamentosa. However, most clinicians would interpret the total picture and not take this facet as determinative in isolation.
Case and photo courtesy of James Bartley, MD
NEXT CASE »
For the discussion, click here.

Case 2:
The results of a skin prick test against a panel of foods in an 11-month-old child are shown. The large erythematous reaction with wheal formation indicates a positive result. The lesion in the lower right of the panel is a reaction to a positive control using histamine.
For a child with persistent or worsening allergy symptoms of more than 2 months’ duration, a screening radioallergosorbent test may be initiated after a careful history and physical examination. Be alert for allergic “shiners” and other signs of allergic disorders in the workup.
Skin testing, performed on the skin of the back, is the most commonly used allergy test. In patients younger than age 2 years with atopic dermatitis, a test for food allergy frequently identifies an offending food. It is prudent to test for indoor allergens in children younger than 5 years and to delay testing for outdoor allergens until age 6 years or older.
Allergy testing can aid the diagnosis of allergic disorders, but it is not diagnostic. With skin testing, in particular, a positive result does not necessarily indicate clinical allergy, and a negative result does not always exclude clinical relevance.
NEXT CASE »
For the discussion, click here.
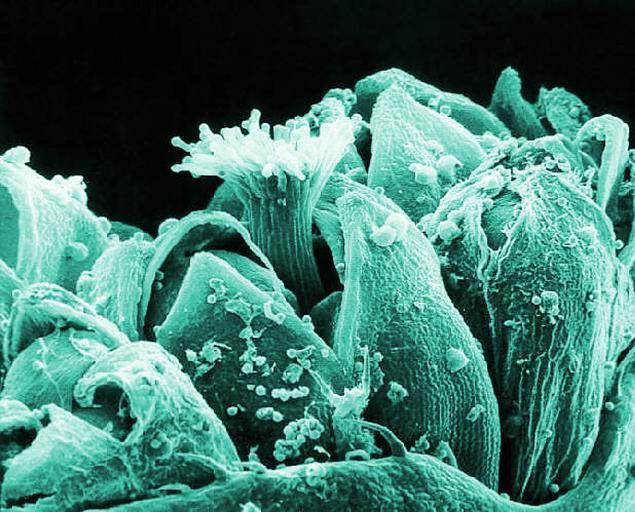
Case 3:
The most common type of asthma is allergic asthma. The most important step in controlling allergen-induced asthma is to reduce exposure to the offending substances, including indoor allergens-such as animal dander, house dust mites, and indoor fungi-and outdoor allergens, such as pollen. A clinician needs to determine the patient’s exposure to allergens and sensitivity to the allergens.
Exposure of vulnerable patients to inhalant allergens increases airway inflammation, airway hyperresponsiveness, symptomatology, need for medication, and incidence of fatal reactions. All patients with asthma should be queried about exposures to these substances and evaluated for allergen sensitivity.
Determining a patient’s relevant inhalant sensitivity will enable you to recommend specific environmental controls to reduce exposure and help the patient understand the pathogenesis of asthma and the value of inhalant allergen avoidance.
NEXT CASE »
For the discussion, click here.

Case 4:
Circumscribed erythematous lesions developed on the back and abdomen of this 19-month-old boy. The rash was mildly pruritic. His parents gave him 1 dose of diphenhydramine, and the rash resolved after an hour. About 12 hours later, new lesions developed on the face, neck, and upper back. He was given the same treatment, and the symptoms resolved. The next morning, widespread lesions were noted on his face, neck, trunk, and extremities.
The recurrent lesions are characteristic of acute urticaria, which may manifest with multiple erythematous wheals anywhere on the body. The lesions can cause mild to intense pruritus. About 20% of the general population have had at least 1 episode of urticaria.
Medications, insect stings, foods, food additives, aeroallergens/contact allergens, transfusion reactions, and infections are common causes.
In a study of children aged 1 to 12 years who had acute urticaria, 90% had concurrent respiratory tract symptoms.
Case and photo courtesy of Elizabeth P. Sternberg, DO
NEXT CASE »
For the discussion, click here.

Case 5:
A 72-year-old woman noted the recent appearance of swelling and itching every time she used her favorite lipstick. She is allergic to an ingredient in the cosmetic.
Lipstick ingredients that may induce allergic reactions include dyes (eosin, carmine), preservatives, metals (bismuth, nickel), and dye solvents (olive oil and others). Patch testing should be performed to determine the specific allergen responsible.
Persistent, rather than episodic, swelling of the lip or lips likely indicates the presence of one of several inflammatory forms of cheilitis.
Case and photo provided by Ted Rosen, MD
NEXT CASE »
For the discussion, click here.

Case 6:
A 63-year-old woman presented with an acute onset of an intensely pruritic, oozing eruption along the hairline, behind the ears, and on the upper face after the first use of a new shampoo.
This history and clinical appearance is quite typical of allergic contact dermatitis of the scalp, most often caused by use of jet black hair dye. Without hair dye use, some ingredient in the new shampoo was likely the culprit.
Cutaneous patch testing would be advisable to pinpoint the offending allergen and facilitate future avoidance. However, the patient refused patch testing.
Case and image courtesy of Ted Rosen, MD
