- Clinical Technology
- Adult Immunization
- Hepatology
- Pediatric Immunization
- Screening
- Psychiatry
- Allergy
- Women's Health
- Cardiology
- Pediatrics
- Dermatology
- Endocrinology
- Pain Management
- Gastroenterology
- Infectious Disease
- Obesity Medicine
- Rheumatology
- Nephrology
- Neurology
- Pulmonology
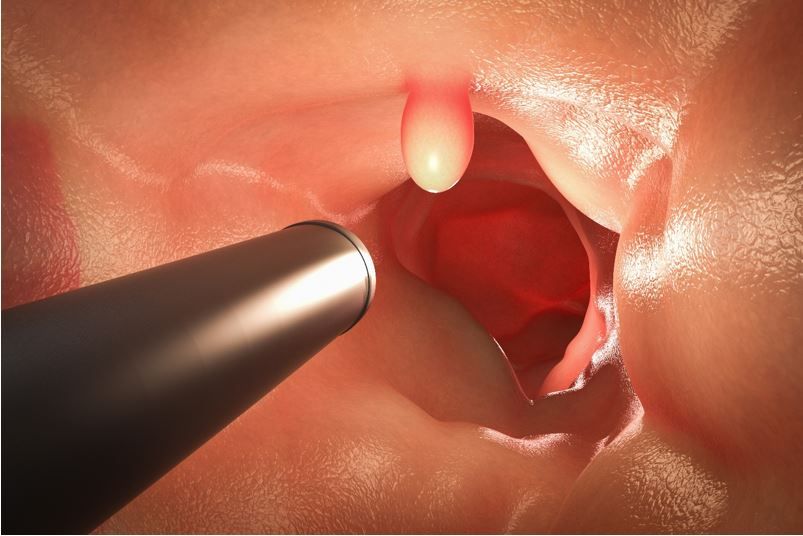
ACP Updates Guidance on Screening for Colorectal Cancer, Maintains Age 50 Years to Start
"Clinicians should start screening for colorectal cancer in asymptomatic average-risk adults at age 50 years," reads Guidance Statement 1 from the American College of Physicians (ACP) updated screening guidance published July 31 in the Annals of Internal Medicine.1
The recommendation to commence screening at age 50 years is consistent with the College's previous guidance and is in conflict with those from current clinical guidelines issued by other professional societies including the American Cancer Society (2018)2 and the US Preventive Services Task Force (2021),3 both of which lowered the age for initial screening in asymptomatic adults to 45 years.
©phonlaimphoto/stock.adobe.com
In considering the risk/benefit ratio of later vs earlier screening, the ACP guidance notes that while CRC incidence has increased slightly among individuals aged 45 to 49 years, it remains much lower than among 50- to 64-year-olds and 65- to 74-year-olds, making the net benefit of screening in adults at average risk in the youngest group less favorable.1
Among dissenting opinions is this, from Richard C. Wender, MD, professor and chair of family medicine and community health at the University of Pennsylvania in Philadelphia, quoted from an interview with Medscape on the topic of the ACP guidance: "The entire nation is now focused on increasing screening capacity and getting everyone screened," he said. "There is not a controversy about age to start, and I anticipate that this paper won't create a new one." Wender also noted in the interview, "While cancer incidence is lower in the 45- to 49-years-old group, the precursors to cancer are present and can be found in a substantial percentage of patients ― the same percentage as 50- to 55-year-olds."4
Guidance Statement 2 says that selection of the type of CRC screening test for the prescribed age group should be based on a shared decision-making discussion between patient and clinician that includes the benefits and harms of the test considered, the cost to the patient, availability of the screening approach, frequency of testing, and the patient's preferences. The ACP evaluated evidence for a range of methods (Figure 1) and recommends that clinicians choose among1 :
- fecal immunochemical or high-sensitivity guaiac fecal occult blood test every 2 years
- colonoscopy every 10 years
- flexible sigmoidoscopy every 10 years plus a fecal immunochemical test every 2 years
Guidance Statement 3 recommends that screening be stopped in adults at average risk older than age 75 years or for whom life expectancy is 10 years or less.
The guidance recommends against using stool DNA, capsule endoscopy, computed tomography colonography, urine, or serum screening tests and continues to support colonoscopy as the gold standard for CRC screening.
Literature review1
ACP based its current guidance on critical review of existing clinical guidelines developed by national-level organizations and published between June 1, 2014, and May 28, 2018, including 3 used commonly in clinical practice (Figure 2). The guidance coauthors also vetted evidence reviews from the 2 guidelines scoring highest on the Appraisal of Guidelines for Research and Evaluation II instrument and from modeling studies used to develop those guidelines where appropriate.
The Clinical Guidance Committee (CGC) stresses that the guidance does not apply to any individual who has long-standing inflammatory bowel disease and those with a family history of CRC.
“This updated guidance will help physicians determine the evidence-based course for their patients for screening for colorectal cancer and to avoid unnecessary screening in this population,” said Omar Atiq, MD, ACP president, in a College news release.5 The CGC does emphasize that CRC screening is not without risks and potential harms that may include cardiovascular and gastrointestinal events (eg, dangerous bleeding, perforation, myocardial infarction, angina), unnecessary follow-ups, and costs for findings deemed clinically unimportant.1
Deficiencies, future research
ACP CGC authors cite the lack of direct comparisons on the effectiveness and harms of the various screening methods, noting that the absence of evidence limits the ability of clinicians to fully educate patients and to better individualize choice of test. Until findings are available from ongoing randomized controlled trials of colonoscopy vs stool-based studies and better evaluations of clinical benefits and harms of FIT plus sDNA and particularly of CT colonography are available, they wrote, “other screening methods have stronger direct and indirect evidence of clinical effectiveness in reducing CRC mortality.”1
There is also a void where information is essential on racial and ethnic disparities, as well as sex differences related to CRC screening and mortality.1
Note from the ACP CGC: "Guidance statements are 'guides' only and may not apply to all patients and all clinical situations. Thus, they are not intended to override clinicians' judgment. All ACP guidance statements are considered automatically withdrawn or invalid 5 years after publication, or once an update has been issued."
