- Clinical Technology
- Adult Immunization
- Hepatology
- Pediatric Immunization
- Screening
- Psychiatry
- Allergy
- Women's Health
- Cardiology
- Pediatrics
- Dermatology
- Endocrinology
- Pain Management
- Gastroenterology
- Infectious Disease
- Obesity Medicine
- Rheumatology
- Nephrology
- Neurology
- Pulmonology
Abnormal Chest X-Ray in a Drug Abuser
A 56-year-old man has been admitted on several prior occasions for left groin abcesses related to injection drug use.
A 56-year-old man has been admitted on several prior occasions for left groin abcesses related to injection drug use. Comorbid disorders include diabetes and tobacco abuse. Recent test results for HIV and TB (PPD test) were negative. On past admissions related to intravenous abuse of heroin and cocaine, the patient was treated with antibiotics and incision with drainage. A CXR and subsequent CT scan, obtained for cough, revealed a left upper lobe nodule. Respiratory isolation was initiated on suspicion of TB.
Examination revealed a chronically-ill appearing man in no distress with the following vital signs: heart rate, 90 beats/min; respiratory rate 14 breaths/min; temperature, 38°C while breathing room air; oxygen saturation, 94%. Auscultation of the heart and lungs was unyielding. Numerous track marks secondary to drug abuse were noted. Serum chemistries, complete blood count, and blood cultures remained negative. Three induced-sputum samples remained negative for bacteria, fungus, and AFB staining. Bronchoscopy was normal and lavage samples failed to identify a pathogen.

Figure 1

Figure 2- Left upper lobe nodule 2.2cm by 1.9cm
Differential diagnoses considered at this point include: TB, primary lung or metastatic neoplasm, granulomatous lung disease (broad differential), aspergilloma, septic emboli, and other pathogens. Thoracoscopic biopsy for definitive diagnosis is shown (Figures 3,4).
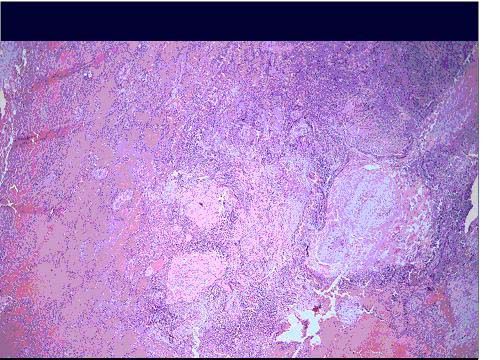
Figure 3
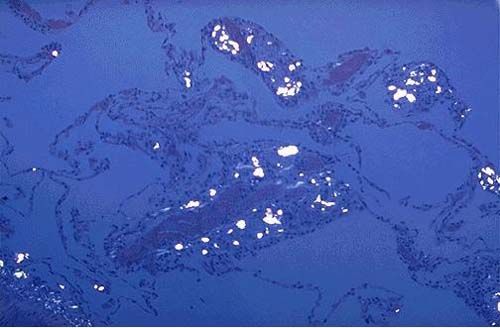
Figure 4
To what diagnosis does the clinical picture point? Answer
Diagnosis: Pulmonary Talcosis
A decision was made to surgically resect the nodule to exclude an early malignant process. The biopsy at low power (Figure 3) demonstrates numerous well-formed granuloma. A high-power view (Figure 4) shows lung tissue with particulate matter (white flecks) deposited within and surrounded by inflammatory cells. Areas of scarring and fibrosis of the interstitium are visible as thick pink areas. Viewed under polarized light, white glowing flecks are visible within the parenchyma, vasculature, and interstitium. These pathological features confirm the diagnosis of pulmonary talcosis. Further clarification of the patient’s drug abuse revealed a history of intravenous injection of opiate tablets.
Discussion
Illicit drug use may be associated with variety of thoracic complications depending on the specific drug used, route of administration, and burden of exposure. Commonly abused drugs that potentially induce thoracic complications include cocaine, opiates, and methamphetamine derivatives. Thoracic complications can be categorized under pulmonary, pleural, mediastinal, cardiovascular and chest wall complications (Table).
Pulmonary talcosis was originally described as a pneumoconiosis associated with mineral worker exposure to talc dust.1 Subsequently, it has been described in a variety of occupations: talc mining and milling, rubber cable manufacture, plate casting, cosmetic manufacture, and textile manufacture.1 In the 1960s, a new form of pulmonary talcosis was described in drug users who chose to abuse oral medications intravenously.2 It is estimated that pulmonary talcosis develops in about 5% of all intravenous drug users.3 Case reports have also described this disease among inhalers of drugs.4
Chemically, talc consists of magnesium trisilicate, and is an important mineral for the industries of ceramics, plastics, and rubber. The pharmaceutical industry employs talc as a ‘filler’ that binds medicinal particles within the tablet. Drug users abuse talc-filled tablets by dissolving in water, filtering with cotton wool, and then injecting the mixture intravenously. Six different medications2 have been reported to be associated with talcosis in addicts: methylphenidate (Ritalin), methadone, tripelennamine (Pyribenzamine), propoxyphene (Darvon), phenmetrazine (Preludin), and amphetamines; all contain talc. The insoluble talc is the culprit that leads to the development of pulmonary disease-- not the drug itself.
The size of the talc particle in the lung can assist in differentiating inhalation from intravenous injection as the source of the talc.5 Inhaled particles are, in general, less than 5 microns in diameter compared with an average particle diameter of 14.2 microns in cases of intravenous talcosis.5 The talc particle is birefringent and forms irregular, plate-like crystals that can be identified under polarization microscopy.
The pathophysiology is not completely understood. The lung acts as a filter for the talc particle, which becomes trapped within pulmonary arterioles and capillaries. Injection of talc-containing drugs results in a foreign body granuloma reaction in the lungs.6 For unclear reasons, widespread granuloma develop in the interstitium of the lung in some patients, while sparing the pulmonary arteries. In others, there is a predominance of granuloma formation in the pulmonary arteries and a sparing of the interstitium.2 It has been proposed that a longer duration of exposure to talc injection is associated with a predominance of granuloma in the interstitium.4
Table – Thoracic complications of illicit drug use
Pneumonia
Pulmonary edema
(cardiogenic/noncardiogenic)
Pulmonary hemorrhage
Aspiration pneumonia
Emphysema
Septic emboli
Pleural/mediastinal
Pneumothorax
Pneumomediastinum
Pneumopericardium
Chest wall
Vertebral body osteomyelitis
Epidural abscess
Necrotizing fasciitis
Costochondritis
Septic arthritis
Cardiovascular
Acute myocardial infarction
Aortic dissection
A number of pathologic findings have been reported. Talc particles afflict the pulmonary vasculature, interstitium, and lung parenchyma. Autopsy evidence for resultant pulmonary hypertension includes right ventricular hypertrophy, medial hypertrophy of muscular pulmonary arteries, fibrous intimal proliferation, and plexiform lesions.2,8 Interstitial lung findings include inflammation and nodular/diffuse fibrosis. In the lung parenchyma, panacinar emphysematous changes that predominate in the lower lobes, has been described. This contrasts with the typical upper lobe emphysematous change observed with tobacco abuse. Lower lobe predomination is hypothesized to be the result of ischemic damage or local leucocyte-induced proteolytic activity.8
Patients with pulmonary talcosis present usually after their fourth decade with non-specific symptoms of cough, wheeze, dypsnea, and hemoptysis.7 Examination may yield crackles or wheeze. Fundoscopy can reveal glistening talc particles concentrated around the macula. Pulmonary function testing commonly shows a reduced diffusion capacity with restriction or obstruction. Late complications include chronic respiratory failure, emphysema, pulmonary arterial hypertension, and cor pulmonale.
Earliest radiological findings are widespread pinpoint nodules on chest films.8 Common CT findings reported in a series of 12 patients included innumerable micronodules (<1 mm), conglomerate masses, ground-glass attenuation, and lower lobe panacinar emphysema.9
Pulmonary talcosis is an irreversible lung disease associated with intravenous abuse of tablets. Abstinence does not appear to arrest the progression of lung disease that is characterized by coalescence of lung nodules resulting in large conglomerates, pulmonary vasculopathy, emphysema, and interstitial fibrosis.8 Treatment is supportive care and consideration for lung transplantation, although recurrence has been reported in one patient after single lung transplant.10
There are an estimated 15.9 million illicit drug users in the United States.11 Intravenous injection is not the usual method of drug abuse. However, this case draws attention to the need for a detailed drug use history and consideration of pulmonary talcosis when faced with a pulmonary nodule in an intravenous drug user.
References:
References
1. Miller A, Teirstein AS, Bader ME et al. Talc Pneumoconiosis. Significance of sublight microscopic mineral particles. Am J Med 1971;50: 395-402.
2. Arnett EN, Battle WE, Russo JV, et al. Intravenous injection of talc-containing drugs intended for oral use. Am J Med 1976;60: 711-718.
3. Roberts WC. Pulmonary talc granulomas, pulmonary fibrosis, and pulmonary hypertension resulting from intravenous injection of talc-containing drugs intended for oral use. BUMC Proceedings 2002;15: 260-261.
4. Oubeid M, Bickel JT, Ingram EA, et al. Pulmonary talc granulomatosis in a cocaine sniffer. Chest 1990;98(1): 237-239. 5. Abraham JL, Brambilla C. Particle size for differentiation between inhalation and injection pulmonary talcosis. Environ Res 1980;21: 94-96.
6. Waller BF, Brownlee WJ, Roberts WC. Self-induced pulmonary granulomatosis. Chest 1980; 78(1): 90-94.
7. Marchioni E, Lourenco S, Gasparetto TD, et al. Pulmonary talcosis: imaging findings. Lung 2010; 188: 165.
8. Paré JP, Cote G, Fraser RS. Long term follow-up of drug abusers with intravenous talcosis. Am Rev Resp Dis 1989;139: 233-241.
9. Ward S, Heyneman LE, Reittner P, et al. Talcosis associated with iv abuse of oral medications: CT findings. Am J Rad 2000;174: 789-793.
10. Cook RC, Fradet G, English JC, et al. Recurrence of intravenous talc granulomatosis following single-lung transplantation. Can Respir J 1998;5: 511-514.
11. Substance abuse and mental health services administration website available at http://oas.samhsa.gov/nhsda. US Department of Health and Health Services. Accessed 2/27/06 .
Common Side Effects of Antiretroviral Therapy in HIV Infection
February 7th 2013What are some of the more common side effects of antiretroviral therapy, and what can the primary care physician do to help manage these effects? In this podcast, infectious disease expert Rodger MacArthur, MD, offers insights and points readers to updated comprehensive guidelines.
