- Clinical Technology
- Adult Immunization
- Hepatology
- Pediatric Immunization
- Screening
- Psychiatry
- Allergy
- Women's Health
- Cardiology
- Pediatrics
- Dermatology
- Endocrinology
- Pain Management
- Gastroenterology
- Infectious Disease
- Obesity Medicine
- Rheumatology
- Nephrology
- Neurology
- Pulmonology
10 Gastrointestinal Upsets, Part 1: A Photo Essay
Ischemic colitis; eosinophilic esophagitis; Crohn disease; necrotizing pancreatitis; diverticulosis: close-up looks and helpful tips here.
Case 1:
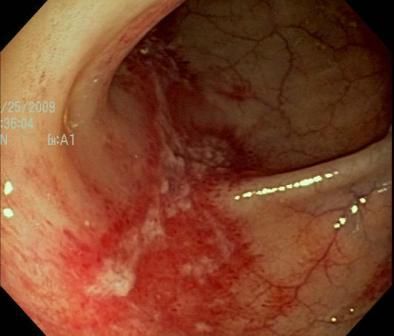
A 62-year-old woman presented after the sudden onset of crampy abdominal pain followed by bloody bowel movements. The results of a screening colonoscopy 12 years earlier had been unremarkable. A CT scan of the abdomen revealed circumferential bowel wall thickening around the region of the descending colon. Now colonoscopy showed a longitudinal ulcer with surrounding inflammation, the single stripe sign. The patient had ischemic colitis.The most susceptible region of the colon is the watershed area (near the splenic flexure). Risk factors include age and atherosclerosis.
Case and image courtesy of Fouad Moawad, MD
NEXT CASE »
For the discussion, click here.
Case 2:
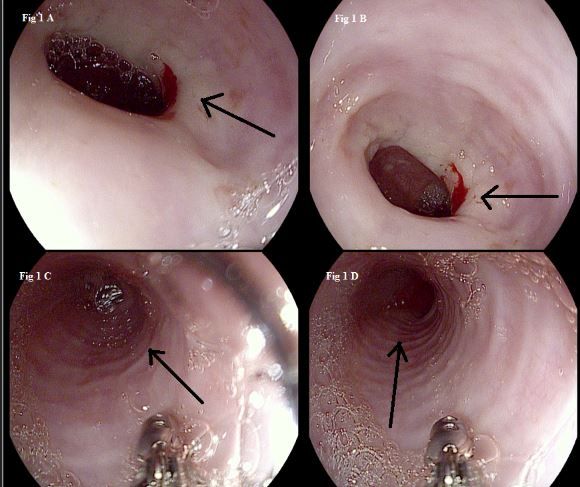
A 44-year-old woman presented with progressive dysphagia for solids, describing a feeling of food getting stuck a few seconds after swallowing. She had associated nausea and vomiting but no fever or weight loss. Endoscopy showed thickened white asymmetrical mucosa at the level of the gastroesophageal junction and felinization, or trachealization, of the esophagus throughout (black arrows). Tissue biopsy of the gastroesophageal junction revealed abundant eosinophils. The findings suggested eosinophilic esophagitis (EoE).
EoE has been recognized increasingly as a major cause of dysphagia, food impaction, and food regurgitation. Typical findings include attenuation of subepithelial vascular pattern, linear furrowing that may extend along the whole length of the esophagus, and surface exudates composed of eosinophils or abscesses or strictures.
Case and images provided by Ranjita Pallavi, MD and Jennifer Harley, MD
NEXT CASE »
For the discussion, click here.

Case 3:
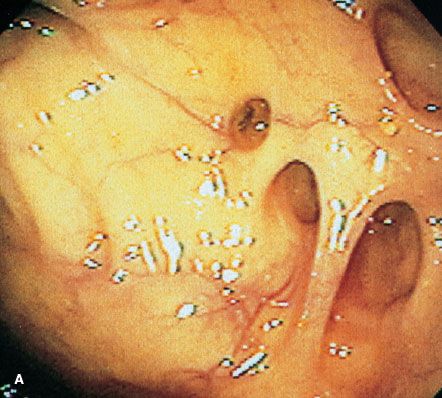
Moderate to severe inflammation typical of Crohn disease is seen in this colonoscopic view of the ileum. Diagnosis of inflammatory bowel disease (IBD) can be obscured by extraintestinal “red herrings”-involvement outside of the bowel that manifests as back pain, joint pain, mouth ulcerations, pyoderma gangrenosum in the legs, or erythema nodosum of the shins.
Here are 5 things to keep in mind about IBD:
1. Delayed diagnosis is common.
2. Look beyond the bowel to the extraintestinal manifestations.
3. Follow the path to diagnosis, and tag team with the specialist.
4. Avoid the prednisone crutch.
5. Keep tabs on bone density and immunizations.
Photo courtesy of David Schwartz, MD
NEXT CASE »
For the discussion, click here.

Case 4:
A 61-year-old obese man with type 2 diabetes mellitus and hypertension presented to the ED with complaints of fatigue, poor oral intake, and weight loss. He denied any significant abdominal pain, nausea, vomiting, steatorrhea, scleral icterus, and jaundice. Imaging revealed acute emphysematous pancreatitis with extensive pancreatic necrosis, without evidence of gallbladder or biliary tract disease.
Necrotizing pancreatitis occurs in up to 20% of patients who have acute pancreatitis. A rare form, emphysematous pancreatitis, is characterized by free air within the lesser sac or pancreatic parenchyma. This typically is attributed to infection rather than an enteropancreatic fistula.
Clinical presentations vary widely, from minimally symptomatic to hemodynamic compromise and shock. Typical are findings classically associated with pancreatitis, including nausea, vomiting, fever, and epigastric pain.
Case and image provided by Michael Chamberlin, MD, Anish Patel, DO, and Cesar Sostre, MD
NEXT CASE »
For the discussion, click here.
Case 5:
Typical lesions of diverticulosis are seen here in the colon of an 84-year-old woman. Diverticula may occur singly or in clusters, with narrow or broad openings into the colonic lumen.
Diverticulosis increases dramatically in incidence with each succeeding decade of life. Patients often are asymptomatic, but abdominal cramps, constipation, and flatulence may mark its presence. Diverticulosis is a major cause of painless rectal bleeding in older patients and may be a presenting complaint. Acute diverticulitis develops in a small percentage of patients.
An increase in dietary fiber or fiber supplements can reduce symptoms in patients who have uncomplicated diverticulosis. Fiber-bulking laxatives may be helpful.
Case and photograph provided by Benjamin J. Marano Jr, MD and Hal J. Freiman, MD
For the discussion, click here.
In part 2, we will describe 5 more common GI disorders.
Clinical Tips for Using Antibiotics and Corticosteroids in IBD
January 5th 2013The goals of therapy for patients with inflammatory bowel disorder include inducing and maintaining a steroid-free remission, preventing and treating the complications of the disease, minimizing treatment toxicity, achieving mucosal healing, and enhancing quality of life.
