- Clinical Technology
- Adult Immunization
- Hepatology
- Pediatric Immunization
- Screening
- Psychiatry
- Allergy
- Women's Health
- Cardiology
- Pediatrics
- Dermatology
- Endocrinology
- Pain Management
- Gastroenterology
- Infectious Disease
- Obesity Medicine
- Rheumatology
- Nephrology
- Neurology
- Pulmonology
Images in HIV-A Photo Essay
Oral lesions, often the harbingers of early HIV infection, rank among the most common complaints for which HIV-positive patients seek primary care. Here we offer visual presentations of these and other lesions associated with HIV.
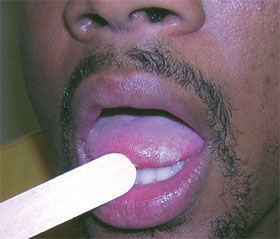
Case 1:
A 30-year-old man with a 15-packyear smoking history presented for a follow-up evaluation of an asymptomatic whitish lesion on the tongue that had not responded to oral therapy with nystatin or fluconazole. Multiple, nontender, whitish, vertical striations were noted along the right lateral edge of the lesion. A presumptive clinical diagnosis was made of oral hairy leukoplakia.
A biopsy was taken and histology revealed hyperkeratosis and koilocytosis without inflammation. Results of the HIV test were positive. The CD4+ cell count was 312/μL. Oral acyclovir was started, and the lesion resolved by the end of the third week of treatment.
Oral hairy leukoplakia is the classic intraoral lesion of HIV/AIDS and is typically asymptomatic. The presentation is almost exclusively seen in men who have sex with men and is generally a sign of moderate to severe HIV disease (with CD4+ cell counts of less than 300/μL). AIDS can be expected to develop in up to 30% of such patients within 3 years.
Case and photo courtesy of James S. Studdiford III, MD and Victor Diaz, MD.
NEXT CASE »
For the discussion, click here.

Case 2:
A 47-year-old HIV-positive man presented with severe thrush, profound dysphagia, and a 30-lb weight loss. He underwent an upper endoscopy with biopsies. Severe esophagitis was seen; biopsy specimens revealed unspeciated Candida. His advanced HIV disease made him vulnerable to the dramatic growth of Candida in his esophagus. He had oroesophageal candidiasis.
Oral candidiasis is the most common fungal infection. Before the advent of highly active antiretroviral therapy (HAART), nearly 90% of patients with HIV infection had oral candidiasis at some point during their illness. Although the development of opportunistic infections, including esophageal candidiasis, is much less common in the post-HAART era, patients with poorly controlled disease are still at high risk.
Topical treatment for oral candidiasis (ie, amphotericin B solution, and miconazole tablets) is not as effective when there is esophageal involvement. Oral systemic therapy includes the azoles, with fluconazole still the most commonly prescribed. The newer echinocandins (glucan synthesis inhibitors) are available only as intravenous treatment.
Case and photo courtesy of Susan C. Ball, MD, MPH, MS
NEXT CASE »
For the discussion, click here.

Case 3:
A 38-year-old openly homosexual man presented with cough and multiple asymptomatic facial lesions. Physical examination showed many small, flesh-colored, umbilicated papules. A chest radiograph was positive for nodular parenchymal infiltrates, most consistent with an infection from either acid-fast bacilli or fungi. The patient refused bronchoscopy.
Hospital screening labs revealed a positive HIV serology and gross lymphopenia. A skin biopsy of a facial papule confirmed disseminated cryptococcosis. Its cutaneous lesions may appear in a wide variety of morphologies. Molluscum-like lesions are quite common; cutaneous cryptococcosis can also simulate cellulitis, panniculitis, Kaposi sarcoma, and non-melanoma skin cancer.
Although the cause of the patient’s pneumonia was not determined, Cryptococcus neoformans is most likely as cryptococcosis can encompass both cutaneous and pulmonary findings. While the fungal infection may lead to harmless colonization of the airways, it may result in disseminated disease in immunocompromised patients.
HIV infection is a specific risk factor for disseminated disease and skin lesions occur in up to 15% of these patients. Cryptococcosis may be the first sign of underlying serious disease. The appearance of secondary cutaneous cryptococcosis portends a poor prognosis; the disease is frequently fatal.
Case and photo courtesy of Ted Rosen, MD
NEXT CASE »
For the discussion, click here.
Case 4:
A 38-year-old African American man with HIV infection presented with numerous dyspigmented macules and patches on the extremities, abdomen, and chest. Initially they were smooth, nontender, and minimally pruritic, but later the skin of his extremities and trunk became intensely pruritic. Pea-sized nodules developed in the areas of chronic scratching, and further itching and scratching led to the pigmentation changes shown here. Prurigo nodularis often occurs in immunocompromised patients, such as those with underlying disorders like HIV infection.
The differential diagnosis of dyspigmented macules and patches in patients with HIV infection includes vitiligo, scabies, bullous pemphigoid, and Kaposi sarcoma. A diagnosis of prurigo nodularis is primarily based on the history and clinical presentation. Laboratory studies (eg, complete blood cell count, metabolic panel) can rule out underlying malignancy and hepatic or renal dysfunction.
Case and photos courtesy of Eric Parks, MD and Girendra Hoskere, MD
NEXT CASE »
For the discussion, click here.
>
Case 5:
A 47-year-old woman who was seropositive for HIV-1 presented to the ED with severe maculopapular, erythematous eruptions. After a change in her antiviral regimen, she developed pruritus, difficulty in swallowing, fever, and painful ulcerations. Scattered target or iris lesions characteristic of erythema multiforme erupted on her trunk, extensor forearms, palms, and soles. Stevens-Johnson syndrome-a severe cutaneous hypersensitivity reaction-was the diagnosis even in the absence of cutaneous bullae.
HIV-1–infected patients are at increased risk for severe mucocutaneous drug reactions. Antiretroviral agents such as zidovudine, didanosine, zalcitabine, and lamivudine are only rarely associated with Stevens-Johnson syndrome. Life-threatening reactions, however, are more commonly provoked by phenolphthalein, phenytoin, ethosuximide, methsuximide, lamotrigine, -lactam antibiotics, and sulfonamides.
The offending agent should not be re-introduced after resolution of symptoms.
Case and photo courtesy of Dr Kamal Boulos, Dr H. Taha, and Dr Gamil Kostandy.
Common Side Effects of Antiretroviral Therapy in HIV Infection
February 7th 2013What are some of the more common side effects of antiretroviral therapy, and what can the primary care physician do to help manage these effects? In this podcast, infectious disease expert Rodger MacArthur, MD, offers insights and points readers to updated comprehensive guidelines.
